Explaining the Health Gap Experienced by Girls and Women in Canada: A Social Determinants of Health Perspective
by Cecilia Benoit, Leah Shumka, Kate Vallance, Helga Hallgrímsdóttir, Rachel Phillips, Karen Kobayashi, Olena Hankivsky, Colleen Reid and Elana Brief
University of Victoria
Sociological Research Online 14(5)9
<http://www.socresonline.org.uk/14/5/9.html>
doi:10.5153/sro.2024
Received: 9 Mar 2009 Accepted: 19 Nov 2009 Published: 30 Nov 2009
Abstract
In the last few decades there has been a resurgence of interest in the social causes of health inequities among and between individuals and populations. This 'social determinants' perspective focuses on the myriad demographic and societal factors that shape health and well-being. Heeding calls for the mainstreaming of two very specific health determinants - sex and gender - we incorporate both into our analysis of the health gap experienced by girls and women in Canada. However, we take an intersectional approach in that we argue that a comprehensive picture of health inequities must, in addition to considering sex and gender, include a context sensitive analysis of all the major dimensions of social stratification. In the case of the current worldwide economic downturn, and the uniquely diverse Canadian population spread over a vast territory, this means thinking carefully about how socioeconomic status, race, ethnicity, immigrant status, employment status and geography uniquely shape the health of all Canadians, but especially girls and women. We argue that while a social determinants of health perspective is important in its own right, it needs to be understood against the backdrop of broader structural processes that shape Canadian health policy and practice. By doing so we can observe how the social safety net of all Canadians has been eroding, especially for those occupying vulnerable social locations.
Keywords: Social Determinants, Sex, Gender, Intersectionality, Health Gap, Canada, Social Location, Life Course
Introduction
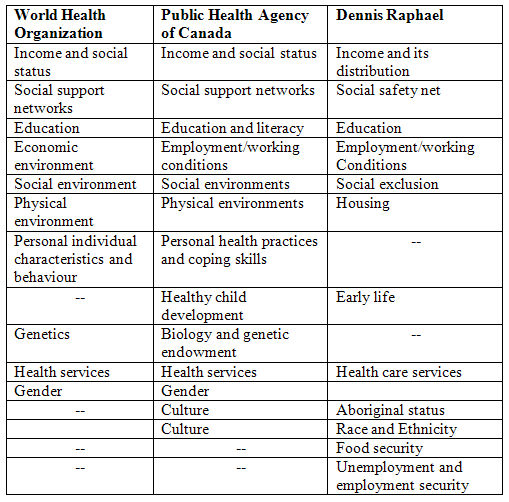
1.1 In the last few decades there has been a resurgence of interest in the social causes of health inequities among and between individuals and populations. This "social determinants" perspective focuses on the myriad demographic and societal factors that shape health and well-being (Glouberman and Millar 2003). At the same time it offers a way to understand inequities in health outcomes among groups by pointing to the layering of genetic and other biological factors with social and cultural factors, which in turn both interact with and shape personal attitudes and behaviours to positively or negatively influence health status (Marmot and Wilkinson 1999; Marmot 2003;Canadian Institute for Health Information 2005; World Health Organization 2008).1.2 Variables or factors commonly understood as determinants include but are not limited to: sex, gender, age, ethnicity, race, education, income, social support, geographical location, and health care access. However, as one can see based on the list provided in Table 1, agencies and researchers differ in their perceptions of what factors constitute social determinants. For example, Canadian researchers, Dennis Raphael and colleagues (2004) emphasize housing, food security, and employment status as vital to the health of Canadians.
| Table 1. Lists of key health determinants by source[0] |
|
1.3 Despite some of the discrepancies concerning what constitutes a social determinant of health, what can be agreed on is that this theoretical perspective aims to identify not merely how these factors individually impact health within a population, but also the reasons why there are differences in health outcomes and how these differences are shaped by an individual's unequal access to key resources. According to Rachlis, "[a] particular population's health status is as unique to that society as fingerprints are to an individual" (2004: 304). What this means is that, while societies may share common traits, each is to some extent differentiated structurally by its unique social, cultural, environmental, economic, political and historical characteristics. Moreover, while genetic and other biological factors help to partially explain variations in health outcomes among individuals, other significant factors include work and social environmental factors and their link to individual behaviour (Wilkinson and Marmot, 2003).
1.4 Some sociologists have gone on to argue that certain social determinants are more "fundamental" than others because of their direct and enduring influence on a range of health outcomes, both locally and globally (Link and Phelan 1995; Coburn 2004; Navarro and Shi 2001; Whitehead, Dahlgren and McIntyre 2007). Link and Phelan (2005) argue specifically that socioeconomic status is the most important factor determining health because access to key resources such as money, power, prestige, and social connections appears to trump all other determinants (e.g., having money and a broad social network can minimize certain health disadvantages related to age, geographic location, or ethnicity). Below we make the case for considering sex and gender as additional fundamental determinants for two reasons. First, there is a dearth of attention paid to sex and gender as determinants of health and, secondly, they too influence one's access to these important social resources. At the same time, we recognize that these fundamental determinants need to be understood within a broader context (Hankivsky and Christoffersen 2008). Therefore, we use an intersectionality approach to show how socioeconomic status, sex, and gender are interconnected with other historically and geographically specific social determinants to create health disparities in Canadians.
Sex and Gender as Fundamental Social Determinants
2.1 Sex has long been considered a factor linked to the health of males and females, although until recently it has been conflated with gender in health research and therefore analyzed relatively uncritically (the reverse is also true whereby gender has been conflated with sex). For this reason, the independent effects of sex and gender on health outcomes, as well as how sex and gender interact and intersect with other determinants, have not been clearly articulated (Lorber 1996). These oversights are based first on a systemic bias among researchers resulting in: 1) the exploration of women's health as an aberration of a health norm historically based on the experience of men; and 2) an inability to disentangle biological and social conditions underpinning health outcomes (Davidson, Kitzinger and Hunt 2006; Doyal 2003).2.2 For these and other reasons feminist health researchers have focused attention in recent decades on bringing sex and gender, especially the unique health concerns of girls and women, to the forefront (Matthews and Beaman 2007). This began with the North American women's health movement in the 1970s and '80s. Until then, explorations of women's health were largely concerned with either reproductive or mental health. At the heart of the feminist health movement was a concern with power and the production and application of scientific knowledge. Women activists sought to take control of the production of health knowledge in order to shed light on women's unique health concerns and, in the process, transform health care and policy. Activists and feminist scholars also joined together to change the male-dominated medical care system by marrying research with action around issues ranging from the legalization of midwives and home birth to women-centred care more generally (Bourgeault, Benoit and Davis-Floyd 2004; DeVries et al. 2001). By highlighting the inequities inherent in a medical and social security system biased towards men's needs, the women's health movement made exploration into women's health legitimate and possible.
Clarifying Sex
2.3 It is generally agreed that sex is a biological construct based on one's sex chromosomes (that is, XX = female, XY = male) and manifested in one's anatomy, physiology, and hormones, and that these attributes tend to be more or less constant across societies (Phillips 2005). Yet the sexes do not fall into two neat dichotomies, a reality that complicates attempts to determine the effect of sex on health. The term intersexual people, for instance, refers to those who have both female and male characteristics. While commonly thought to be quite rare, with Fausto-Sterling reporting in 1985 that only one infant in every 1000 is born in North America with ambiguous genitalia, Hester (2003) more recently indicates that as many as 1.7 intersexed infants are born per 100 each year (Blackless, Charuvastra, Derryck, Fausto-Sterling, Lauzanne and Lee 2000). Substantial numbers of intersexual people are born each year in Canada with some combination of male and female genitals, and no specific pattern applies to all. Yet as a culture we are most comfortable with sex as a binary, evident in the demand placed on parents to record the sex of their new born as either female or male on their birth records. Historically, this has been mirrored in the push from health professionals to surgically assign these individuals a single sex, so that in turn they can be assigned a definitive gender (i.e., masculine or feminine). As Katrina Karkazis states, "[c]ultural understandings of categories such as male and female and ideas about appropriately gendered subjects drive treatment decisions about intersexuality" (2008: 11). While some cultures are more open to accepting intersex people as "normal", sometimes attributing to them special abilities, the binary model of sex is hegemonic in Anglo-western countries and parents who choose not to seek medical treatment for their intersexed child are often socially stigmatized and isolated. What this reveals is that the current standard treatment of intersex is shaped by historical and cultural forces that are intricately linked to gender (Karkazis 2008).
2.4 At the same time there is a relatively high incidence of asymptomatic people with sex chromosome anomalies (e.g., Turner's syndrome [XO] and Klinefelter Syndrome [XXY], among others). As well, secondary sex characteristics, such as a person's amount of facial hair, breast size, and hormone levels, vary greatly within populations. For instance, although testosterone is a hormone usually associated with males, it is found to greater and lesser degrees in both males and females, depending on their age, health status, and use of pharmaceutical drugs. Further, according to Johnson, Greaves and Repta, female and male bodies "respond differently to alcohol, drugs, and therapeutics due to differences in body composition and metabolism, as well as differences in hormones" (2007:4).
2.5 While the majority of people can be "classified" into either male or female sex-based categories and, for the most part, do exhibit distinct physiological differences, what this evidence suggests is that we need to move past binary distinctions. At the same time, it points to the difficulty of determining patterns of health and illness based on sex (Lorber 1993). As Verbrugge noted two decades ago: "[t]he single greatest need in population studies of sex differences in health and mortality is operational measures of that biological substrate" (1989: 296). In other words, is it possible to accurately measure sex as a biological category, distinct from gender? Nevertheless, it is important to consider sex a fundamental determinant of health because it has repeatedly been found to be an important predictor of both the incidence and severity of diseases that affect the human population (Wizemann and Pardue 2001). Sex should thus be considered as a basic variable in health research and such studies should consider sex differences beginning in the womb and over what sociologists refer to as the "life course". Improvements in our ability to accurately measure sex differences would only refine and further nuance our understanding of associated patterns in morbidity and mortality. Equally important, however, is articulating how sex differs from gender, being careful not to conflate the two as genetic/biological and social/cultural distinctions place very different demands on health-based therapies and treatments and policy-based interventions.
Clarifying Gender
2.6 Many researchers agree that our biological sex is made even more complicated by our gendered selves (Rubin 1975; Lorber 1996; Krieger 2003); that is, those qualities, characteristics, mannerisms, and behaviours that are deemed as either masculine or feminine according to varying cultural norms and values. Gender includes the socially mediated roles and norms typically enacted and ascribed to women, men, and other gender groups (e.g., transgendered, two-spirited[1], and queer) that change over time, place, and stage in life (Oakley 2000). In Canada, as in most parts of the world, all aspects of life are gendered in some way, from the colours we wear, the alcoholic beverages we imbibe, the sports we play, to the career paths we follow. While seemingly innocuous and perhaps mundane, gender as a dimension of social organization shapes our access to material and symbolic resources, how we interact with others, and even how we think about ourselves (Matthews and Beaman 2007). Gendered norms also shape experiences of illness, what health care problems come to the attention of researchers and get investigated, what health services are made available through the public purse, and the norms and values influencing patient care (Riska and Wegar 1993; Spitzer 2005). Research in the addictions field, for example, has shown how gender roles can influence interpretations of and patterns in substance use, whereas complementary research in the area of sex has revealed how biological factors influence the impact of substances on the body (Bureau of Women's Health and Gender Analysis 2005).
Can We Separate Sex and Gender in Terms of their Effect on Health?
2.7 There is contradictory evidence about whether sex and gender separately or in combination result in differences in health between men and women (Annandale and Hunt 1990; Lahelma, Arber, Martikainan, Rahkonen and Silventoinen 2001). On the one hand, if we focus our attention on the role of sex, some have argued that females enjoy a natural biological advantage over males from early on in the life course because female fetuses are less likely to abort spontaneously (Wizemann and Pardue 2001). There are also a wider variety of genetically predisposed diseases that afflict males (e.g., haemophilia or Duchene Muscular Dystrophy). We also know that, in high-income countries at least, females tend to live longer than males. This may also be explained, in part, by differences based on gender. For example, men are more likely to be employed in physically dangerous jobs such as mining, logging, and fishing. Historically, men have also been more likely to work or volunteer in the military and participate in more aggressive and/or individualistic activities that have been shown to be risky and dangerous (e.g., contact sports and race car driving). The result is higher rates of mortality for men in most high-income countries as a result of accidents, interpersonal violence, and suicide (Möller-Leimkühler 2003). Some researchers argue this is because men are socialized to take physical risks, exhibit bravery, and avoid emotional expression — what Kimmel (2006) sees as a form of "hegemonic masculinity" and what Riska (2002) characterizes as the "hardy man" model.
2.8 Parallel studies argue that women experience greater morbidity than men. For example, the lifetime prevalence of major depression for women in Canada is double that of men, and women are also more prone to experience stress caused by life course events (Stephens, Dulberg and Joubert 1999). Women in the US are twice as likely as men to be given a diagnosis of unipolar depression, anxiety, panic disorder, and agoraphobia, and three times more likely to be diagnosed with a borderline personality disorder (Kessler and Magee 1993). Recent Canadian research also shows that, when other risk factors are taken into account, depression is significantly associated with an increased risk of heart disease among females. For reasons still unknown, this is not the case among males experiencing depression (Gilmour 2008).
2.9 Explanations for this kind of sex/gender disparity have been noted by some as the result of biases in diagnostic processes as well as the diagnostic criteria themselves. This argument suggests that men and women are equally as likely to suffer morbidity due to illness and disease, but that health is interpreted differently based on gender, with women more likely to be diagnosed as being sick or ill. Women's mental and emotional problems, for instance, have historically tended to be medicalized as is evident in the proliferation of hysteria diagnoses in the 19th century. Yet this continues today with the proliferation of "syndromes" that are thought to especially afflict women (e.g., Chronic Fatigue Syndrome, Premenstrual Syndrome, Menopause and Fibromyalgia) (Davis 1996; Kaufert and Gilbert 1986; Närvänen 2002; Rapping 1996; Ware 1992). This is in contrast to men who have been, and continue to be, encouraged not to talk about their mental and emotional concerns and to ignore any physical ailments. Annandale and Hunt (1990) suggest that this is a result of stereotypical notions linking femininity with dependency, weakness, and poor mental and emotional health and masculinity with independence, strength, stoicism and robust health, although allowing for some physical concerns.
2.10 Some researchers argue it is an "urban myth" that there are unchanging or universal gender differences in health (MacIntyre, Hunt and Sweeting 1996). Providing a more nuanced and context-specific analysis, they suggest the influence of sex and gender on men and women's health depends, at a minimum, on the time period, country, health indicator and age of the participant group (Arber and Cooper 2000; Lahelma et al. 2001; Annandale and Hunt 2000). Canadian research lends support to this literature, showing variation in gender differences in health over time, as well as in comparative perspective (Benoit 2000; McDonough and Walters 2001; Denton, Walters and Prus 2004).
2.11 What this debate indicates is that sex and gender may – singularly and together – impact the health of men and women differently. There is no evidence of a universal pattern of gender differences and both factors intersect with other determinants to cause particular health outcomes that vary across time and place. We use the term intersect here purposefully to refer to intersectionality which is both a theory and method which explicitly focuses on differences among groups and seeks to illuminate various and interacting social factors that affect individuals' lives, including social locations[2], health status, and quality of life (Hankivsky 2005; Iyer, Sen and Ostlin 2008). Intersectionality thus seeks to understand what is created and experienced at the intersection of two or more axis of diversity on the basis that it is precisely at an intersection that a completely new social location, that is more than simply the sum of its individual parts, is formed (Varcoe, Hankivsky and Morrow 2007). The essential insight of intersectionality theory is that various dimensions of social stratification—including sex and gender but also socioeconomic status, ethnicity, race, and so on—can add up, or culminate, to great disadvantage for some categories of people. Thus, an individual's genetic endowment and biological heritage interact with their sex and gender statuses as well as their location in society's stratification system to produce their particular health status (Mechanic 2000; Denton et al. 2004; Nazroo 2003). Intersectionality is also an advancement in that it starts to reveal the true complexity of people's lives and how social locations interact with each other (instead of simply layering or prioritizing).
Dimensions of the Health Gap Experienced by Girls and Women in Canada
3.1 What this discussion of the intersectionality emphasizes is a need for a context specific approach (Wrede, Benoit, Bourgeault, Van Teijlingen, Sandall and DeVries 2006), one that is careful not to conflate sex and gender while also taking into consideration some of the other reported factors determining the health of women and girls in Canada, including socio-economic status, race, ethnicity, immigrant status, geographic location, and employment status and security. To be meaningful, all these must be viewed through a political and economic lens, taking into consideration, as Canadian researcher Dennis Raphael (2006) does, the ways in which historical, political, and economic processes have shaped Canadian health policy and practice and led to the slow erosion of Canadians' social safety net, leaving certain populations especially vulnerable to health inequities. It is important to note, that while each of the following sections focus on a different health determinant, none are mutually exclusive and all intersect and overlap with others in formative ways to influence the health of Canadians.Socioeconomic Status (SES) Inequities
3.2 As noted above, recognition of how inequities in health are associated with SES —as measured by education, occupation, and income —is one of the main contributions of the social determinants perspective. Mackenbach and colleagues reported inequities in morbidity across SES groupings in ten western European countries during the 1980s (Mackenbach, Kunst, Cavelaars, Groenhof and Geurts 1997). A more extensive study examining the link between SES and health inequities in twenty-two European countries since 1995 confirmed and extended the authors' original findings (MacIntyre and Ellaway 2000). Individuals with less education, which is a key marker of low SES, were found to have higher rates of death from all causes except breast cancer. With respect to mortality rates associated with cardiovascular disease, one-third of deaths among males and one-half of those among females have been linked to education-related inequities (MacIntyre and Ellaway 2000). Researchers refer to this phenomenon as the "opportunity structure" through which people who are privileged gain access to health-enhancing physical environments (e.g., clean water and quality food and shelter), access to a local configuration of resources (such as good schools, safe and high-quality childcare centres, better-equipped recreation facilities), and social environments that foster social support and community participation (Armstrong 2004). While differences in this opportunity structure are clearly evident between males and females, it is equally necessary to recognize its salience for understanding inequities between groups of females as well.
3.3 Being in the highest income category is an important predictor of good health for Canadian women (Denton and Walters 1999). Canadian women from low-SES backgrounds on the other hand are more likely to smoke, be overweight, live in unsafe neighbourhoods, maintain greater or sole responsibility for child and/or elder care, and perform substantial amounts of unpaid domestic labour (Janzen 1998; Spitzer 2005). The fact that it is economically privileged females who, through the purchase of paid help, frequently employ poor females at the bottom of the opportunity structure (Seguin et al. 1999) suggests that there are structures of power in place whereby the health advantage of more privileged females is supported by the labour of their lower SES counterparts. The social location of lower-income women instead exposes them to a broader range of physical and psycho-social health concerns, including muscle strains and injuries, anxiety, stress, and maternal health concerns such as postpartum depression (Fromer 1988; Gottleib 1988; Zeytinoglu, Denton and Davies 2002).
3.4 This is not to say that high-SES protects females from all health concerns. Better-off girls and women are, for example, more vulnerable to endometriosis (Fromer 1988) —which is the presence of uterine lining in other pelvic organs and characterized by cysts and long and/or painful menstruation. This is related to higher use of estrogen-based birth control, later age at first birth of children, and dieting during sexual maturation among higher-income females (Fromer 1988). However, health concerns such as this are less pervasive and also less likely to threaten the overall health, safety, and security of those affected, which is not the case for females who are less well off and overburdened with more serious health problems.
3.5 Low-SES, or economic marginalization, places Aboriginal women in Canada at a particular disadvantage compared to women who are relatively better off. Approximately 70 percent of women working in the Vancouver's Downtown Eastside (DTES) as sex workers are Aboriginal. Some of the reasons why Aboriginal women are particularly likely to work in the sex industry are due to their lower levels of education which result in fewer job opportunities and poverty. As Currie (1995) tells us, Aboriginal women living in the DTES are often without a high school education and the majority have three or more children. Teen births are 13 times higher in the DTES than in other regions of Vancouver. Other statistics indicate that one-half of all Aboriginal families are headed by lone mothers and 80 percent of Aboriginal children in the urban ghetto live in poverty. These are powerful motivating factors for women to make money any they way can. What is especially troubling, however, is that these Aboriginal women have increased morbidity and mortality compared to their non-Aboriginal counterparts living and working in the same areas. Some of the most common health concerns are sexually transmitted infections including HIV/AIDS.
Inequities and Race, Ethnicity, and Migrant Status
3.6 Race, a socially constructed category that classifies people based on a constellation of biologically shared traits such as skin colour, facial features, hair texture, and body shape, can be associated with the incidence of certain forms of diseases such as sickle cell anaemia. At the same time, there is often an intersection between a person's race and their ethnicity —a group's shared cultural heritage based on common ancestry, language, music, food, and religion. Both can lead to vulnerabilities to certain social determinants of health (e.g., poverty, stigma, and/or marginalization) and can, in combination, give rise to specific health disadvantages for certain groups of people. In the case of Canada's Aboriginal peoples, for example, rates of diabetes are three to five times higher than those of the general Canadian population (Young, Moffatt and O'Neil 1993). While genetic explanations related to race (the so-called "thrifty gene theory") is often posited as a possible explanation for this marked disparity, confounding this are factors related to ethnicity such as the historical marginalisation of Aboriginal people in Canada and how poverty and government policies have resulted in dramatic changes to their traditional diet and food harvesting activities (Dickason 1992).
3.7 Despite progressive changes to Canadian immigration policy over the past few decades (since the introduction of the Points System in 1967) and the enactment of legislation like the 1985 Multiculturalism Act, ethnic inequalities in population health and health care are two domains in which differences across and within groups are evident (Kobayashi, Prus and Lin 2008). Recent research attempting to disentangle the effects of immigrant status and ethnicity has found that for visible minority Canadians, e.g., South Asians and Chinese, immigrant status matters. Indeed, it can be reasoned that first-generation adults in these two groups may face specific health issues related to the stress, anxiety, and physical difficulties associated with transitioning from culturally familiar home to uncharted foreign environments (Kobayashi, Prus and Lin 2008). However, of particular relevance to this paper is that immigrant status and ethnicity intersect to create patterns of disadvantage among women. As a case in point, recent research highlights the importance of this intersection for understanding the epidemiology of breast cancer among women in Canada. While early detection leads to favourable prognosis and improved health outcomes, breast self-exam, clinical breast exams, and screening mammography programs are generally underutilized by visible minority women. For example, Ahmad and Stewart (2004) studied breast cancer among South Asian women, who are the largest and fastest growing category of new immigrant women in Canada. The authors found that these women underutilize screening programs partly based on the belief they are at a low risk since the incidence of breast cancer is comparatively low in their country of origin. Such a belief has been maintained despite a significant body of recent research on the healthy immigrant effect (Gee, Kobayashi and Prus 2004). The healthy immigrant effect maintains that new immigrants experience a health advantage when they first immigrate, but that they lose this advantage over time as they adopt mainstream beliefs, attitudes, and lifestyle behaviours (e.g., smoking, dietary changes, increased alcohol consumption). Research in this area also shows that there are entrenched patriarchal structures that lead many immigrant women to neglect their own health, particularly breast cancer screening. This neglect arises from their obligation to fulfill multiple responsibilities that range from continuous care of children and frail older adults to sole responsibility for cooking and cleaning at home. Compounding this problem are inadequate financial resources for transportation and other costs (e.g., payment for childcare) associated with going to the doctor. Finally, cultural barriers play a role in that both self-exams and clinical assessments challenge ethno-cultural beliefs related to the appropriateness of self-touching or being touched by a doctor of the same or opposite gender (Ahmad, Cameron and Stewart 2005). These findings indicate the need for multi-collaborative, culturally sensitive cancer-screening programs that emphasize specialized training for health-care providers on the specific needs and concerns of visible minority immigrant women over the life course.
Inequities in Employment Security
3.8 Employment is an important determinant of health and is linked to income and the ability to purchase health-enhancing resources such as nutritious foods, shelter, health services, and recreational activities. What is more, for some Canadians, employment comes with health and safety benefits and provides a social safety net in the form of employment insurance and pension benefits. However, this is only true if one has a "good" job, that is, one that is full-time, secure, and offers the benefits mentioned above. In the current global economic climate, many of the Canadians who might be considered lucky enough to be employed have what Winson and Leach (2002) characterize as "bad" jobs, i.e., contingent or precarious jobs which are often short-term or part-time in nature and characterized by fewer hours, lower skill requirements, little or no health or dental benefits, substantially lower wages, and a greater likelihood of being laid off or fired. Not surprisingly, it is women who are the most likely to hold contingent jobs (Benoit 2000; Armstrong and Laxer 2006). While women are more likely to have contingent work – often in the service sector - recent Canadian evidence indicates that men are harder hit in economic recession because male dominated industries such as construction and manufacturing tend to recede more than services (Statistics Canada 2009).
3.9 Taking a closer look at one form of contingent service work, the literature on home-care workers – a job that includes performing personal and household services from bathing, dressing, and monitoring the health of older adult clients in their own homes, to doing their cooking, cleaning, and shopping (Aronson and Neysmith 1996) – provides a compelling example of how work is also highly gendered. The poor compensation, little or no health benefits, unsafe working conditions, unregulated hours, and discrimination that can define home care work helps maintain health inequities among certain groups of women (Aronson and Neysmith 1996; Zeytinoglu, Denton and Davies 2002). In both Canada and the United States, these relatively undesirable jobs are held by lower-income, ethnic and immigrant women.
3.10 Recent US and Canadian research indicates that as many as 80 percent of home-care workers are women and that within this group there is an "over-representation of racial and ethnic minorities" as well as immigrants (Bureau of Labor Statistics 2003; Stacey 2005: 836). These women earn near-minimum-wage and must be willing to accept part-time and/or other contingent work arrangements in order to secure a job. The physical costs associated with the job are frequently high in that both home-care workers and home-nursing aides "suffer from the highest number of musculoskeletal disorders of any occupational group in the US" (Stacey 2005: 843). This is partly a result of the strain associated with transporting and manoeuvring frail and/or immobile clients. Research from Canada reports similar findings (Zeytinoglu et al. 2002; Denton, Zeytinoglu, Webb and Lian 1999).
3.11 The emotional impact of care work for an aging population can also be high. Some workers have found it difficult to forge the necessary interpersonal relationships with their clients in order to make it feasible to work in their homes under highly intimate circumstances. On the other hand, some workers find themselves overly investing in their clients' well-being, especially those who are poor in health, lonely, and as financially constrained as the home-care workers themselves. Stacey (2005) found that when home-care workers too closely identify with their clientele, these workers tend to work unpaid overtime to keep lonely or scared clients company, perform duties beyond their skill level and training (e.g., provide medical care), and/or drive their clients to/from doctors' appointments (potentially making the worker liable). These varied tasks can place care workers in a compromised economic position and be emotionally taxing, which increases their psychological distress and burnout. While it is important to emphasize that there are many rewards associated with care work —such as autonomy, skill building, and dignity that come with providing a much-needed service —it is clear that low SES intersects with gender (as well as race, ethnicity, and immigrant status) to constrain the opportunities and health status of women in this line of work (Zeytinoglu et al. 2002; Denton et al. 1999).
Inequities and Geographic Location
3.12 As noted above, the Canadian population is dispersed over a vast landscape that varies widely in natural resources and infrastructure. Approximately 80 percent of Canadians reside in urban areas of 10,000 or larger and the remaining 20 percent live in smaller towns or villages. It is not surprising, then, that the health of Canadians is also highly contingent on the place where they reside. As our example of Aboriginal women living in Vancouver's Downtown Eastside highlights, there are marked differences in health based on whether one lives in a high- or low-income neighbourhood of a city or town (CIHI 2006).
3.13 The connection between place and health is also evident when we consider the differences between urban and rural settings—those living in more isolated geographic areas face greater disadvantage due to the lack of both economic and social resources. As a recent Canadian study, How Healthy are Rural Canadians? (CIHI 2006a) reveals, health decreases the farther a person resides from a major urban centre. This can be especially true for rural women who have significantly higher mortality rates than urban women (DesMeules, Manual and Cho 2003; Dolan and Thien 2008). A combination of factors are at play, including lower educational achievement and lower labour force participation among rural women as compared to those living in urban centres. Rural women also tend to have higher fertility rates and more high-risk pregnancies, to report greater stress, anxiety, depression, domestic/interpersonal violence, and to smoke (Dolan and Thien 2008; Lee and Lutz 2005; Morrow, Hankivsky and Varcoe 2004; Stout, Kipling and Stout 2001; Varcoe and Irwin 2004). According to Dolan and Thien:
Certain subsets of rural women are considered especially vulnerable, including Aboriginal, elderly and disabled women. In Canada, Aboriginal women die younger, and suffer higher rates of violence, substance abuse, suicide, and chronic diseases (e.g., arthritis, hypertension, heart problems, diabetes) compared to non-Aboriginal women; a result, in part, of the significant challenges of living in rural and northern communities (2008: S38).
3.14 Recent research in northern British Columbia exemplifies precisely how and why Aboriginal women living in rural and remote locations might find themselves especially vulnerable to these and other health concerns. Varcoe and Dick (2008) conducted research looking at the "intersecting dynamics" of gender, rural living, race, and poverty for determining women's risk of violence and exposure to sexually transmitted diseases (STIs) and HIV. The majority of the women in the study had experienced multiple forms of abuse and these experiences were "compounded by poverty, drug and/or alcohol use and limited access to support services, all of which put them at significant risk for exposure to HIV and other sexually transmitted infections (STIs)" (Varcoe and Dick 2008: 44). For many women, the lack of career opportunities and limited resources in rural locations forced them to stay in abusive relationships for the conditional economic security they provided. Others were compelled either by these abusive partners or by their dire economic circumstances into unwanted or unprotected sex, and this in turn left them at an increased risk of contagious infections. Due to systemic racism and the "neocolonial context of Canadian society," rural and on-reserve Aboriginal women were particularly likely to find themselves in these difficult situations. The legacy of residential schools and the associated loneliness and despair associated with being separated from friends and family, losing language and traditional culture, and sexual, physical, and emotional abuse (Browne and Fiske 2001; Browne and Smye 2002), has shaped rural Aboriginal women's lives in very distinct ways and left many vulnerable to drug and alcohol misuse and entering and staying in abusive relationships.
3.15 Geographic isolation and the realities of living in economically depressed outlying regions also means that women residing there often lack access to the educational, childcare, and other services and resources that could help them improve their lives. Instead,
many of the participants talked about how they had to move to urban centres for education and employment opportunities, better health care, greater anonymity, and safety from various forms of violence. This both disconnected the women from their support networks and depleted human resources in the rural area (Varcoe and Dick 2008: 48).
3.16 Further, government cuts in health and social services, including legal aid and social assistance, mean these women either have to leave their communities where they have no social support or they are compelled to remain in abusive relationships. Funding cuts to these regions also means less education and fewer prevention programs for violence and HIV, fewer street nurse services to address immediate health concerns, and fewer women's centres and support groups (Dolan and Thien 2008; Hanlon and Halseth 2005).
3.17 At the same time that resource-related funding cuts have limited the social services available to many women living in rural and remote regions of Canada, the federal and provincial governments have been "down-sizing health care services, broadly characterized in rural communities by centralization of services (e.g., maternity care, rural hospital, bed and clinic closures), privatization of services (e.g., more fee-for-service models of care) and shifting responsibility for services to the community level (e.g., deinstitutionalization of care)" (Dolan and Thien 2008: S40). As a result, pregnant women living in rural and remote locations in Canada face a particular set of health challenges due to the lack of maternity care services (Centre for Rural Health Research 2008). This shortage forces rural and remote women to travel to major urban centres to give birth in regional hospitals. For many women, this means paying out-of-pocket costs for travel, food, and lodging while they are away. While some women may decide to stay home and have unassisted home births for financial and social support reasons, they too can run into trouble if they find they have a difficult labour or encounter any unexpected health emergencies. One possible solution to this problem is more and better-trained midwives available throughout the province, perhaps working in concert with nurse-practitioners (CIHI 2004). However, due to a host of obstacles (see Benoit, Carroll and Westfall [2007] for an in-depth discussion), such remedial actions seems unlikely. As a result, rural pregnant women, but Aboriginal women in particular, are in the unenviable situation where there are too few physicians to tend to their prenatal and childbirth needs, publicly funded midwives are too few in numbers and generally located in urban centres, and the biomedical establishment lacks the cultural sensitivities to appropriately train women who want to live and work in their own communities.
Summary and Conclusions
4.1 With this paper we have drawn on the social determinants of health perspective and largely Canadian research by feminist and other scholars on sex and gender in order to better understand the health gap experienced by girls and women in Canada. We drew on the theory of intersectionality as it offers a conceptual framework to combine these literatures when attempting to understand inequities in health among particular populations and is positioned as a more nuanced and sophisticated way to approach the determinants of health. We focused on the intersection between some of the most important dimensions of the observed health gap experienced by girls and women in Canada – socioeconomic status, race, ethnicity, immigrant status, employment and geographical location. Our findings suggest that certain groups of girls and women in Canada face a formidable cumulative disadvantage. This is particularly the case for those who are poor, of Aboriginal background or visible minority status, foreign-born, or reside in rural areas. However, other pivotal factors identified by social determinants of health scholars, including education, age, social support networks and sexual orientation, intersect with the determinants indentified above and thus are also worthy of attention and, indeed, have been shown to have a significant cumulative impact on health over the life course (Navarro and Shi 2001; Raphael 2006; Whitehead, Dahlgren and McIntyre 2007).4.2 Failing to examine sex and gender as fundamental health determinants that intersect with other mitigating factors homogenizes the experiences of women (and men), reifying existing inequities while at the same time overlooking important sources of within-group variation (Annandale and Hunt 2000; Butler 1990; Whittle and Inhorn 2001). As Janzen succinctly points out, "the determinants of women's health are no doubt complex . . . likely arising from a combination of interacting economic, social, psychological, and biological forces" (1998: 34).
4.3 It is worth reminding ourselves about the key message of the social determinants of health perspective, namely, that the maintenance and promotion of a population's health is only partly achieved by public investment in health services such as hospitals, physicians, and advanced medical technology (Marmot and Wilkinson 2000; Rachlis 2004; Public Health Agency of Canada 2004). According to the World Health Organization (2008), we could close the health gap within and across countries in the next decade if, in addition to improving access to primary health care, we take concerted action on reducing the health gap caused by the intersection of fundamental factors, including sex and gender, as well as socioeconomic status, race, ethnicity, immigrant status, employment and geographical location. Progressive changes in the Canadian context that are likely to reduce such inequity include an increase in the minimum wage for private as well as public sector employment, equal pay for work of equal value, policies to raise the value of care work that is predominantly performed by girls and women, establishment of a national childcare system, public funding for care of the disabled and elderly, improved educational and economic opportunities for Aboriginal peoples, ethnic minorities and new immigrants, and, of course, increased investment in primary health care in an effort to improve health care access and quality of care for its vulnerable populations, including girls and women in rural and remote areas as well as the inner city.
Notes
1 Two-spirited is a term common among North American and Canadian First Nations indigenous groups to refer to people who dress and carry out roles of both men and women.2 Social location refers to the multiple "roles" or "statuses" that one individual can occupy at any given time. It is, in large part, conditioned by an individual's age, sex, gender, ethnicity, health-status, sexual orientation and occupation. Individuals can move in and out of various social locations as the circumstances of their lives change (Shumka 2006).
References
AHMAD F., D.E. Stewart. 2004 "Predictors of clinical breast examination among South Asian immigrant women." Journal of Immigrant Health 6(3):119-126.
AHMAD, F., J.I. Cameron and D.E. Stewart. 2005. "A tailored intervention to promote breast cancer screening among South Asian immigrant women." Social Science and Medicine 60: 575-586. [doi:10.1016/j.socscimed.2004.05.018]
ANNANDALE, E. and K. Hunt. 1990. "Masculinity, femininity and sex: an exploration of their relative contribution to explaining gender differences in health." Sociology of Health & Illness 12: 1-24. [doi:10.1111/1467-9566.ep10844865]
ANNANDALE, E. and K. Hunt. 2000. Gender inequalities in health. Buckingham: Open University Press.
ARBER, S. and H. Cooper. 2000. "Gender and inequalities in women's health across the life course." PP. 123–149 in Gender Inequalities in Health, edited by E. Annandale and K. Hunt. Buckingham: Open University Press.
ARMSTRONG, P. 2004. "Health, social policy, social economies, and the voluntary sector." Pp. 331-342 in Social determinants of health: Canadian perspectives, edited by D. Raphael. Toronto: Canadian Scholars' Press.
ARMSTRONG, P. and K. Laxer. 2006. "Precarious work, privatization, and the health care industry: The case of ancillary workers." Pp. 115-140 in Precarious employment: Understanding labour market insecurity in Canada, edited by L. Vosko. Montreal & Kingston: McGill-Queen's University Press.
ARONSON, J. and S.M. Neysmith. 1996. "You're not just in there to do the work: Depersonalizing policies and the exploitation of home care worker labor." Gender and Society 10: 59-77. [doi:10.1177/089124396010001005]
BENOIT, C. 2000. Women, Work and Social Rights: Canada in Historical and Comparative Perspective. Scarborough, Ontario: Prentice Hall Canada.
BENOIT, C., D. Carroll and R. Westfall. 2007. "Women's Access to Maternity Services in Canada: Historical Developments and Contemporary Challenges." Pp. 507-27 in Women's Health in Canada: Critical Theory, Policy and Practice, edited by Varcoe, C., O. Hankivsky, and M. Morrow. Toronto: University of Toronto Press.
BLACKLESS, M., A. Charuvastra, A. Derryck, A. Fausto-Sterling, K. Lauzanne and E. Lee. 2000. "How Sexually Dimorphic are We?" American Journal of Human Biology 12(2): 151-166. [doi:10.1002/(SICI)1520-6300(200003/04)12:2<151::AID-AJHB1>3.0.CO;2-F]
BOURGEAULT, I., C. Benoit and R. Davis-Floyd (Eds.). 2004. Reconceiving midwifery. Montreal and Kingston: McGill-Queen's University Press.
BROWNE, A.J. and J. Fiske. 2001. "First Nations women's encounters with mainstream health care services." Western Journal of Nursing Research 23(2): 126-147. [doi:10.1177/019394590102300203]
BROWNE A.J. and V. Smye. 2002. "A postcolonial analysis of health care discourses addressing Aboriginal women." Nurse Research: The International Journal of Research Methodology in Nursing and Health Care 9(3): 28-41.
BUREAU OF LABOR STATISTICS. 2003. Table 11: Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity. Household Data Annual Averages. U.S. Department of Labor.
BUREAU OF WOMEN'S HEALTH AND GENDER ANALYSIS. 2005. Girls, women, substance use and addiction. Ottawa: The Women's Health Policy Program.
BUTLER, J. 1990. Gender trouble: Feminism and the subversion of identity. New York: Routledge.
CENTRE FOR RURAL HEALTH RESEARCH. 2008. "Geographic induction: Time for a protocol." Pp. 104 in Policy Brief, Issues in Rural Maternity Care Series, 3.1. Vancouver, BC.
CIHI (Canadian Institute for Health Information). 2004. Giving birth in Canada: A regional profile. Ottawa, ONT.: CIHI.
CIHI (Canadian Institute of Health Information). 2006. Improving the Health of Canadians: An Introduction to Health in Urban Places. Ottawa, ONT.: CIHI.
CIHI (Canadian Institute of Health Information). 2006a. How Healthy Are Rural Canadians? Ottawa, ONT.: CIHI.
COBURN, D. 2004. "Beyond the income inequality hypothesis: Class, neo-liberalism, and health inequalities." Social Science and Medicine 58: 41-56. [doi:10.1016/S0277-9536(03)00159-X]
CURRIE, S., S.N. Laliberte, N. Bird, N. Rosa and S. Sprung. 1995. Assessing the violence against street involved women in the downtown Eastside/Strathcona community. Vancouver BC: Ministry for Women's Equality, Downtown Eastside Youth Activities Society (DEYAS), and Watari Research Society.
DAVIDSON, R., J. Kitzinger and K. Hunt. 2006. "The wealthy get healthy, the poor get poorly? Lay perceptions of health inequalities." Social Science and Medicine 62: 2171-2182. [doi:10.1016/j.socscimed.2005.10.010]
DAVIS, D. 1996. "The Cultural Constructions of the Premenstrual and Menopause Syndrome." Pp. 57-86 in Gender and Health: an International Perspective, edited by C.F. Sargent, and C.B. Brettell. New Jersey: Prentice-Hall, Inc.
DENTON, M. and V. Walters. 1999. "Gender differences in structural and behavioral determinants of health: an analysis of the social production of health." Social Science & Medicine 48: 1221-1235. [doi:10.1016/S0277-9536(98)00421-3]
DENTON, M., I. Zeytinoglu, S. Webb and J. Lian. 1999. "Occupational Health Issues among Employees of Home Care Agencies." Canadian Journal on Aging 18:154-181.
DENTON, M., I. Zeytinoglu, S. Davies and J. Lian. 2002. "Job Stress and Job Dissatisfaction of Home Care Workers in the Context of Health Care Restructuring." International Journal of Health Services, 32 (2), 327-357. [doi:10.2190/VYN8-6NKY-RKUM-L0XW]
DENTON, M., V. Walters and S. Prus. 2004. "Gender Differences in Health: A Canadian study of the Psychosocial, Structural and Behavioural Determinants of Health." Social Sciences and Medicine 58: 2585-2600. [doi:10.1016/j.socscimed.2003.09.008]
DESMEULES, M., D. Manual and R. Cho. 2003. "Mortality, life and health expectancy of Canadian women." Pp. 1-8 in Women's health surveillance report: A multidimensional look at the health of Canadian women, edited by DesMeules M., and D. Stewart. Ottawa: Canadian Institute for Health Information.
DEVRIES, R., C. Benoit, E. R. van Teijlingen and S. Wrede (Eds). 2001. Birth by Design: Pregnancy, Maternity Care, and Midwifery in North America and Europe. New York: Routledge.
DICKASON, O. 1992. Canada's First Nations: A History of Founding Peoples from Earliest Times. Toronto, ONT.: McCelland and Stewart.
DOLAN, H. and D. Thien. 2008. "Relations of Care: A Framework for Placing Women and Health in Rural Communities." Canadian Journal of Public Health 3(3): 569-579.
DOYAL, L. 2003. "Sex and gender: The challenges for epidemiologists." International Journal of Health Services 3: 569-579. [doi:10.2190/CWK2-U7R6-VCE0-E47P]
FROMER, M.J. 1988. The endometriosis survival guide: Our guide to the latest treatment options and the best coping strategies. Oakland, CA: New Harbinger.
GEE, E.M., K.M. Kobayashi and S.G. Prus. 2004. "Examining the healthy immigrant effect in mid- to later life: Findings from the Canadian community health survey." Canadian Journal on Aging 23(Supplement 1): S61-S69. [doi:10.1353/cja.2005.0032]
GILMOUR, H. 2008. "Depression and risk of heart disease." Pp. 1-11, edited by Statistics Canada. Retrieved June 21, 2009 (http://www.statcan.gc.ca/pub/82-003-x/2008003/article/10649-eng.htm).
GLOUBERMAN, S. and J. Millar. 2003. "Evolution of the determinants of health, health policy, and health information systems in Canada." American Journal of Public Health 93: 388-392. [doi:10.2105/AJPH.93.3.388]
GOTTLEIB, A. 1988. "American premenstrual syndrome: A mute voice." Anthropology Today 4:10-13. [doi:10.2307/3032946]
HANKIVSKY, O., and A. Christoffersen. 2008. "Intersectionality and the determinants of health: a Canadian perspective. Critical Public Health [serial online] 18: 271-283. [doi:10.1080/09581590802294296]
HANKIVSKY, O. 2005. "Gender vs. Diversity Mainstreaming: A Preliminary Examination of the Role and Transformative Potential of Feminist Theory." Canadian Journal of Political Science 38(4): 977-1001. [doi:10.1017/S0008423905040783]
HANLON, N. and G. Halseth. 2005. "The greying of resource communities in Northern British Columbia: Implications for health care delivery in already under-serviced communities." The Canadian Geographer 49(1): 1-24. [doi:10.1111/j.0008-3658.2005.00077.x]
HESTER, D. 2003. "Rhetoric of the Medical Management of Intersexed Children: New insights into "Curing", "Illness" and "Healing"." Genders 38: online journal.
IYER, A.,G.Sen and P.Ostlin. 2008. "The intersections of gender and class in health status and health care." Global Public Health 3: 13-24. [doi:10.1080/17441690801892174]
JANZEN, B.L. 1998. Women, gender and health: A Review of the recent literature. Winnipeg, MB: Prairie Women's Health Centre of Excellence. Retrieved June 21, 2009 <http://www.pwhce.ca/womenGenderHealth.htm>).
JOHNSON, J., L. Greaves and R. Repta. 2007. Better science with sex and gender: A primer for health research. Vancouver: Women's Health Research Network.
KARKAZIS, K. 2008. Fixing Sex: Intersex, Medical Authority, and Lived Experience. Durham, NC: Duke University Press.
KAUFERT, P. and P. Gilbert. 1986. "Women, Menopause, and Medicalization." Culture, Medicine and Psychiatry 10: 7-21. [doi:10.1007/BF00053260]
KESSLER, R.C. and W.J. Magee. 1993. "Childhood adversities and adult depression: Basic patterns of association in a U.S. National Survey." Psychological Medicine 23: 679-690. [doi:10.1017/S0033291700025460]
KIMMEL, M.S. 2006. "'What about the boys?' What the current debates tell us- and don't tell us about boys in school." Pp. 361-375 in Reconstructing Gender: A Multicultural Anthology, edited by E. Disch. Boston, MA: McGraw Hill.
KOBAYASHI, K.M., S.G. Prus, and Z. Lin. 2008. "Ethnic Differences in Self-Rated and Functional Health: Does Immigration Status Matter?" Ethnicity and Health 13: 129-147. [doi:10.1080/13557850701830299]
KRIEGER, N. 2003. "Genders, sexes, and health: What are the connections—and why does it matter?" International Journal of Epidemiology 32.
LAHELMA, E., S. Arber, P. Martikainen, O. Rahkonen and K. Silventoinen. 2001."The Myth of Gender Differences in Health: Social Structural Determinants across Adult Ages in Britain and Finland." Current Sociology 49: 31-54. [doi:10.1177/0011392101049003004]
LEE, J. and J. Lutz. 2005. Situating "race" and racisms in space, time and theory. Kingston & Montreal: McGill-Queen's University Press.
LINK, B.G. and J. Phelan. 1995. "Social conditions as fundamental causes of disease." Journal of Health and Social Behavior 35: 80-94. [doi:10.2307/2626958]
LINK, B.G. and J. Phelan. 2005. "Fundamental sources of health inequalities." Pp. 71-84 in Policy challenges in modern health care, edited by D. Mechanic, L.B. Rogut, D. Colby, and J Knickman. Piscataway, NJ: Rutgers University Press.
LORBER, J. 1993. "Believing is Seeing: Biology as Ideology." Gender & Society 7: 568-581. [doi:10.1177/089124393007004006]
LORBER, J. 1996. "Beyond the binaries: Depolarizing the categories of sex, sexuality and gender." Sociological Inquiry 66: 143-159. [doi:10.1111/j.1475-682X.1996.tb00214.x]
MCDONOUGH, P. and V. Walters. 2001. "Gender and health: reassessing patterns and explanations." Social Science & Medicine 52(4): 547-59. [doi:10.1016/S0277-9536(00)00159-3]
MACINTYRE, S., K. Hunt and H. Sweeting. 1996. "Gender differences in health: Are things really as simple as they seem?" Social Science & Medicine 42(4): 617-24. [doi:10.1016/0277-9536(95)00335-5]
MACINTYRE, S. and A. Ellaway. 2000. "Ecological approaches: Rediscovering the role of the physical and social environment." Pp. 332-348 in Social Epidemiology, edited by L.F. Berkman and I. Kawachi. New York: Oxford University Press.
MACKENBACH, J.P., A.E. Kunst, J.M. Cavelaars, F. Groenhof and J.J. Geurts. 1997. "Socioeconomic inequalities in morbidity and mortality in Western Europe." Lancet 349: 1655-1659. [doi:10.1016/S0140-6736(96)07226-1]
MARMOT, M. and R. G. Wilkinson (Eds.). 1999. The Social Determinants of Health. Oxford: Oxford University Press.
MARMOT, M. and R. G. Wilkinson. 2000. Social Determinants of Health. Oxford University Press, Oxford.
MARMOT, M. 2003. "Understanding social inequalities in health." Perspectives in Biology and Medicine 46(3): S9-S23.
MATTHEWS, B. and L. Beaman. 2007. Exploring Gender in Canada. Toronto: Prentice Hall.
MECHANIC, D. 2000. "Rediscovering the Social Determinants of Health." Book Review Essay. Health Affairs, 19(3): 269-276. [doi:10.1377/hlthaff.19.3.269]
MÖLLER-LEIMKÜHLER A. 2003. "The gender gap in suicide and premature death or: why are men so vulnerable?" European Archives of Psychiatry and Clinical Neuroscience 253: 1-8.
MORROW. M., O. Hankivsky and C. Varcoe. 2004. "Women and Violence: The effects of dismantling the welfare state." Critical Social Policy 24: 358-384. [doi:10.1177/0261018304044364]
NÄRVÄNEN, A.L. 2002. "Women's Experiences of Stigma in Relation to Chronic Fatigue Syndrome and Fibromyalgia." Qualitative Health Research 12(2): 148-160.
NAVARRO, V. and L. Shi. 2001. "The political context of social inequalities in health." Social Science and Medicine 52: 481-491. [doi:10.1016/S0277-9536(00)00197-0]
NAZROO, J. Y. 2003. "The Structuring of Ethnic Inequalities in Health: Economic Position, Racial Discrimination, and Racism." American Journal of Public Health 93(2): 277-84. [doi:10.2105/AJPH.93.2.277]
OAKLEY, A. 2000. Experiments in knowing: Gender and method in the social sciences. Cambridge, MA: Polity.
PHILLIPS, S. 2005. "Defining and measuring gender: A social determinant of health." International Journal for Equity in Health 4: 1-4. [doi:10.1186/1475-9276-4-11]
PUBLIC HEALTH AGENCY OF CANADA. 2004. "The social determinants of health: An overview of the implications for policy and the role of the health sector." Retrieved June 26, 2007 <http://.phac-aspc.gc.ca/ph-sp/ou-ar/pdf/01_overview_2.pdf>).
RACHLIS, M. 2004. "Health care and health." Pp. 297-310 in Social determinants of health: Canadian perspectives, edited by D. Raphael. Toronto: Canadian Scholars' Press.
RAPHAEL, D. (Ed.). 2004. Social determinants of health: Canadian perspectives. Toronto: Canadian Scholars' Press.
RAPHAEL, D. 2006. "Social determinants of health: Present status, unanswered questions, and future directions." International Journal of Health Services 36: 651-677. [doi:10.2190/3MW4-1EK3-DGRQ-2CRF]
RAPPING, E. 1996. The Culture of Recovery: Making Sense of the Self-Help Movement in Women's Lives. Boston: Beacon Press.
RISKA, E. and K. Wegar (Eds.). 1993. Gender Work and Medicine: Women and the Medical Division of Labour. London: Sage Publications.
RISKA, E. 2002. "From type A man to the hardy man: Masculinity and health." Sociology of Health and Illness 24: 347-358. [doi:10.1111/1467-9566.00298]
RUBIN, G. 1975. "The Traffic of Women: Notes on the Political Economy of Sex." Pp. 157-210 in Towards an Anthropology of Women, edited by R. Reiter. New York: Monthly Review Press.
SEGUIN, L., L. Potvin, M. St-Denis, and J. Loiselle.1999. "Socio-environmental factors and postnatal depressive symptomatology: A longitudinal study." Journal of Women's Health 29: 57-72.
SHUMKA, L. 2006. "Working through the Body: Women, Pain, and the Embodiment of Work." Unpublished Masters Thesis, University of Victoria, Victoria, BC.
SPITZER, D. 2005. " Engendering health disparities." Canadian Journal of Public Health 51(Supplement 2): S78-S96.
STACEY, C.L. 2005. "Finding dignity in dirty work: The constraints and rewards of low-wage home care labour." Sociology of Health and Illness 27: 831-854. [doi:10.1111/j.1467-9566.2005.00476.x]
STATISTICS CANADA 2009 The Daily: Latest Release From Labour Force Survey, Posted September 4, 2009 <http://www.statcan.gc.ca/subjects-sujets/labour-travail/lfs-epa/lfs-epa-eng.htm> Last Accessed Sept 10, 2009.
STEPHENS, T., C. Dulberg, and N. Joubert. 1999. "Mental health of the Canadian population: A comprehensive analysis." Chronic Diseases in Canada 20: 118-126.
STOUT, M., G. Kipling and R. Stout. 2001. Aboriginal women's health research: Synthesis report. Ottawa: Centres of Excellence for Women's Health, Women's Health Bureau, Health Canada. Pp. 1-43.
VARCOE, C. and S. Dick. 2008. "The intersecting risks of violence and HIV for rural Aboriginal women in a neo-colonial Canadian context." Journal of Aboriginal Health 4(1): 42-52.
VARCOE, C. and L. Irwin. 2004. ""If I killed you, I'd get the kids." Women's survival and protection work with child custody and access in the context of woman abuse." Qualitative Sociology 27(1): 77-99.
VARCOE, C., O. Hankivsky and M. Morrow (Eds.). 2007. Women's Health in Canada: Critical Theory, Policy and Practice. Toronto: University of Toronto Press.
VERBRUGGE, L. 1989. "The Twain Meet: Empirical Explanations of Sex Differences in Health and Mortality." Journal of Health and Social Behavior 30: 282-304. [doi:10.2307/2136961]
WARE, N.C. 1992. "Suffering and the Social Construction of Illness: The deligitimation of Illness Experience in Chronic Fatigue Syndrome." Medical Anthropology Quarterly 6(4): 347-361. [doi:10.1525/maq.1992.6.4.02a00030]
WHITEHEAD, M., G. Dahlgren and D. McIntyre. 2007. "Putting equity center stage: Challenging evidence-free reforms." International Journal of Health Services 37: 353-261. [doi:10.2190/B296-826U-6VH8-0U82]
WHITTLE, K.L. and M. Inhorn. 2001. "Rethinking difference: A feminist reframing of gender/race/class for the improvement of women's health research." International Journal of Health Services 31: 147-165. [doi:10.2190/FKJA-CXD7-V4G6-U4W9]
WILKINSON, R. and M. Marmot (Eds.). 2003. Social Determinants of Health: The Solid Facts .Copenhagen: World Health Organization. Retrieved June 21, 2009 <http://www.euro.who.int/document/e81384.pdf>). WINSON, A. and B. Leach. 2002. Contingent Work, Disrupted Lives: Labour and Community in the New Rural Economy. Toronto: University of Toronto Press.
WIZEMANN, T.M. and M.-L. Pardue (Eds.). 2001. Exploring the Biological Contributions to Human Health: Does Sex Matter? Washington, DC: Board on Health Sciences Policy, Institute of Medicine.
WHO (World Health Organization). 2008. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health. Geneva, Switzerland: WHO.
WREDE, S., C. Benoit, I. Bourgeault, E. Van Teijlingen, J. Sandall and R. DeVries. 2006. "Decentred Comparative Research: Context Sensitive Analysis of Maternal Health Care." Social Science & Medicine 63: 2986-2997. [doi:10.1016/j.socscimed.2006.07.011]
YOUNG, T.K., M.E.K. Moffatt and J.D. O'Neil. 1993. "Cardiovascular diseases in a Canadian arctic population." American Journal of Public Health 83:88 1-887.
ZEYTINOGLU, I., M. Denton and S. Davies. 2002. "Casual Jobs, Work Schedules and Self-reported Musculoskeletal Disorders among Home Care Workers." Women Health and Urban Life 1: 4-24.