A Critical Analysis of the Medical Model as used in the Study of Pregnancy and Childbirth
by Edwin van Teijlingen
University of Aberdeen
Sociological Research Online, Volume 10, Issue 2,
<http://www.socresonline.org.uk/10/2/teijlingen.html>.
Received: 9 Jan 2004 Accepted: 11 Jan 2005 Published: 30 Jun 2005
Abstract
One key concept in medical sociology/anthropology for the analysis of approaches to health and illness is the medical model. However, this medical model is not only applied at the analytical level, i.e. as a sociological tool, but it also appeals to health service providers at a practical level as a model of working practice. This paper challenges the uncritical use of the medical model by practitioners and social scientists alike.
The purpose of this paper is to separate and analyse the three different levels of understanding expressed in any model of childbirth, whether medical or social: (1) the practical; (2) the ideological and (3) the analytical level. Social scientists are advised to reflect on the question: 'At what level am I using the medical model as a theoretical concept in my work?' This is necessary not only to avoid further confusion, but also to ensure that our sociological tools maintain their ability to analyse the social world appropriately, without becoming 'blunt' due to the uncritical use.
Keywords: Birth, Childbirth, Medical Model, Medical Sociology, Midwifery, Pregnancy, Risk, Medicalisation, Social Model
Introduction
1.1 Analysing approaches to health and illness in terms of a 'medical' versus a 'social' model, henceforth 'the medical model', is a key concept in both medical sociology and medical anthropology (e.g. Chang and Christakis 2002; Helman 1985; Lowis and McCaffery 1999; Lichtman 1999). This medical model is part of the wider conceptual framework of 'medicalisation'. The latter is a process of social change; it can be seen as a change over time from a social model to a more (bio-)medical model. Conrad and Schneider (1980) suggested that medicalisation can take place at three levels: (1) the conceptual; (2) the institutional; and (3) the practitioner-patient level. More recently, Lowis and McCaffery (1999: 26-29) argued that the medicalisation of midwifery may be examined within a sociological framework at five levels: (1) technological; (2) conceptual; (3) interactional; (4) control; and (5) gender status level. If medicalisation occurs at three or five levels, it is highly unlikely that one single 'medical model' is applicable at all these levels. Nevertheless, the notion of a medical model itself is still being used fairly indiscriminately and uncritically in both the social science and the midwifery literature.One model, three levels
2.1 The medical model is not only applied as an academic tool at the analytical or conceptual level, it also appeals to health care practitioners at a practical level. Thus it is not uncommon to find comments in the midwifery literature indicating that the medical model was clearly not purely an analytical tool, but related to actual ways of practice, for example: 'midwives are rejecting the medical model of birth and are developing distinctive ways of practice ...' (Fleming 1998: 137), or 'the patriarchal biomedical model ... is no longer appropriate. There is now increasing pressure to implement a more participatory model of caring ...' (Stapleton 1997: 63). In New Zealand Shaw (2002: 145) noted "a shift in women's choice of Lead Maternity Carer from the medical model to midwifery care". Or the medical model itself is 'doing something', for example Edwards (2000: 74-5) referred to '...certain choices, such as having a breech baby at home, were considered by the medical model to be inappropriate.' Confusion arises when a way of practice is then treated as an exemplar that should be copied elsewhere, and is thus used as a basis for arguments advocating a particular pattern of working practices or deploring others. This phenomenon is in itself very understandable, since the distinction between a medical and social model is (a) simple and easy to understand for non-sociologists unlike some sociological theory; and (b) appealing to those challenging professional medical dominance. The latter, often in conjunction with patient-centred care, has its roots in the consumer movement as well as the women's movement.Aims and objectives
3.1 This paper aims to disentangle the three different levels of understanding expressed in the medical model: (1) practical; (2) ideological; and (3) analytical level. This methodological analysis will offer sociologists some methodological clarification, and provide them with adequate tools for conceptualising and analysing structural processes.Background: Models of health care as applied to childbirth
4.1 Over the past four decades the medical model has often been applied in studies of maternity care, midwifery and childbirth (e.g. Oakley 1979, 1980, 1984; Nash and Nash 1979; Rooks 1983; Comaroff 1977; Lumey 1993; Rothman 2001), and related areas such as infertility (Becker and Nachtigall 1992). Although the medical model has long been applied to other health fields, for example, obesity (Chang and Christakis 2002), health education (Kelly et al. 1997), disability (Oldman 2002), mental health (Gerard 1999;Child 2000) or addiction (Barrows 1998; May 2001), the medical model appears to be especially applicable to childbirth and maternity care. As pregnancy and birth are 'biological and physiological events which are very much embedded in a social and cultural setting' (Van Teijlingen 2003: 120), these are good examples to highlight the use and misuse of the medical and social model. According to Rosengren (1962: 371): 'Pregnancy seems to be controversial in terms both of its social meaning as well as its medical implications.' Or, in the words of Comaroff, (1977: 116), 'Pregnancy in western society, in fact, straddles the boundary between illness and health: the status "pregnant" is unclear in this regard and women perceive that others are not sure whether to treat them as ill or well.' Most medical specialities dealing with the physical aspect of the human body do not give rise to the same fundamental controversy, since the 'pure' illness character of their field is more straight forward, hence more generally recognised, which in turn legitimates medical intervention and control. As Davis-Floyd (1987: 491) stated: 'Obstetrics, unlike other medical specialties, does not deal with true pathology in the majority of cases it treats: most pregnant women are not sick.' The notion that pregnancy and childbirth are not diseases, also influences the accompanying perception of inherent risk. People's concern about risk in childbirth reflects the link between parenthood and social identity, as well as deriving from awareness of the possibility of death or injury to mother or baby. One of the central elements of the divergence between these models relates to the definition of what constitutes a tolerable or acceptable risk (e.g. Lane 1995: 56). Thus defining the risk in childbirth has further implications for the organisation of maternity care, both for the place of delivery and for the preferred birth attendant.
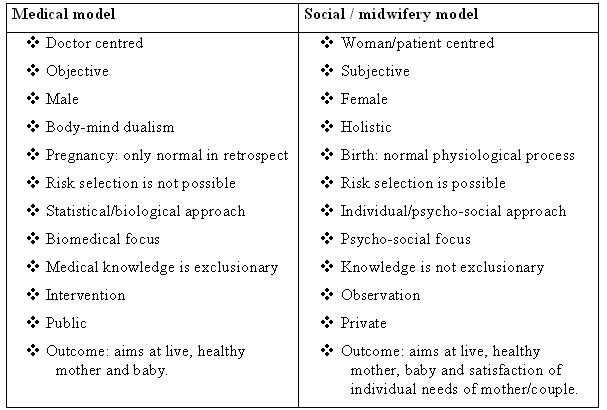
|
(Sources: Bryar 1995; Davis-Floyd 1987; Gillespie and Gerhardt 1995: 83; Helman 1985; Oakley 1999: 321; Porter 1999: 135; Rooks 1999; Van Teijlingen and Bryar 1996; Wagner 1994).
4.2 Table 1 lists the two schools of thought, one stresses its possible medical risks, and the other emphasises that pregnancy is a normal life event. The school of thought adhering to the medical model is founded on the idea that 'normal' childbirth requires medical control in order to guarantee safety through monitoring which will enable intervention at the earliest sign of pathology, since risk prediction and selection is not really possible. The school adhering to the social model is founded on the idea that 'normal' childbirth is 'natural' childbirth, i.e. that the overwhelming majority of pregnant women have a normal and safe childbirth with little or no medical intervention, and that those women who are not expected to have a 'normal' childbirth can be predicted and selected out. Savage (1986: vxi), herself an obstetrician, expressed both views succinctly: 'Pregnancy is not an illness. ... every pregnancy is normal unless there are indications that something is wrong. Those at the opposite end of the obstetric spectrum believe that no pregnancy is normal, except in retrospect.' However, this is not the only distinction between these schools of thought. Differences of definition exist at the level of working practice, at the level of real people organising their work, pregnant women attending antenatal clinics, and so on. Thus schools of thought are more than just abstract and academic; they are associated with concrete and practical ways of doing things. Different groups of maternity care providers operate differently because they employ different working practices. Conceptually, the two levels at which one can approach the controversy about pregnancy, the analytical and the practical, are quite distinct. There is, of course, a third aspect to either of the contrasting schools of thought, namely an ideological one. At the ideological level, practitioners and supporters of a particular model seek to justify their actions, and claim control over certain aspects of childbirth, and claim absolute or 'authoritative' knowledge (Davis-Floyd and Sargent 1997). Thus the US 'medical view of birth as potential pathology ... is a powerful and dominant model' (Lazarus 1997: 134) and 'this dominant ideology of medically controlled birth as "normal" birth envelops women's thoughts about their own births and the use of technological interventions' (Lazarus 1997: 135).
Separating models of childbirth
5.1 In order to avoid confusion about the different usage of the phrases 'medical' and 'social' model of childbirth, this paper reserves different terms for the working practice, its ideology, and the analytical approach. These levels need to be kept separate in a sociological analysis, since it is too easy to fall into the trap of confusing the working practice and the ideology of the practitioners with the corresponding analytical approach. Table 2 suggests three levels at which one might consider these different approaches to childbirth. As part of the confusion is due to applying the same nametag, i.e. medical model, to all three levels, two of these levels have been renamed for clarity in Table 2.
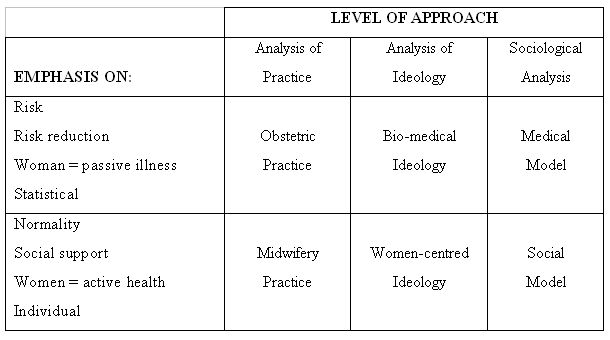
|
Practice or operational level
6.1 At the practical or empirical level the focus is on what people do in their daily lives, for example, as maternity-care practitioners or as health-service users. However, it is recognised that at the level of practice the medical model has been put forward as one of many, adding to the confusion around it. For example, Cronenwett and Brickman (1983) outlined the medical model as one of four possible models of helping and coping in childbirth. They recognise (1) a moral model which attributes to people responsibility (and blame) for both creating and solving problems; (2) a compensatory model which does not blame people for their problems, but holds them responsible for solving them; (3) a medical model which holds people responsible neither their problems nor the solution; and (4) a enlightenment model which blames people for their problems, but does not hold them responsible for solutions (Cronenwett and Brickman 1983).6.2 For the sake of argument this paper dichotomises the medical and the social model. Thus the description of the working practice can be couched in terms of a contrast between an obstetrical practice and a midwifery practice. The former represents the general ways of working of medical practitioners, of midwives and obstetric nurses following their directions in specialist obstetrics units. The latter represents the general ways of working of practitioners in the community and small community maternity hospitals. Both are applicable regardless of gender, occupational background or job title. Thus midwives can be seen to operate according to an obstetric practice as ward sisters in a specialist obstetric hospital, or, in accordance with a midwifery practice, as midwives in the community. It can also be used at a service provision level, for example Wagner (1994: 7) commented that: 'examining health services for birth has propelled WHO (World Health Organization) into the conflict between medical and social models of health.' Comaroff (1977: 131) noted that the different ways of practice with their 'contrasting perspectives are expressed in contrasting rituals relating to pregnant women.' In practice, a whole range of combinations of the two ways of operating can be seen. In terms of a scale from a total obstetrical practice to a total midwifery practice, all working practice is somewhere in between. DeVries (1993:132) commented on this range of practice: 'If we organized midwives along a continuum, with those who use all the tools of modern technology at one end and those who are non-technological in orientation at the other, those on the extreme ends of the continuum would not recognize each other as members of the same occupation.' The distinction between obstetric and midwifery practice is therefore purely analytic, in the sense that the working practice of, for example, a particular midwife, doctor or maternity unit is subject to negotiation.
Obstetrical practice
7.1 In obstetrical practice, pregnancy is regarded as a medical process. One of the underlying motives for this approach might be that 'One important norm within the culture of the medical profession is that judging a sick person to be well should be more avoided than judging a well person to be sick' (Graham and Oakley 1986: 101). Pregnancy is now considered as potentially pathological in the industrialised world (e.g. Arney 1982; Oakley 1984;Kloosterman 1978: 86; Killus 1984: 110). The pregnant woman comes to be viewed in mechanistic terms almost as an object. In Rothman's (1982: 84) words: 'Birthing women are thus objects upon whom certain procedures must be done.' This practice is based on a science-oriented perspective, whereby risk is defined as statistical risk, and whereby solutions and improvements are based on measurements of outcome through mortality and morbidity statistics. Pregnant women are labelled as 'high risk' on the basis of statistical, rather than individual considerations.7.2 The technological orientation of large obstetric hospitals dominated by male doctors has transformed the midwife's role to that of a handmaiden of technocrats (Benoit 1989: 172). A similar development is analysed in nursing by Freidson (1970: 20-2). One of the consequences of change in midwifery, combined with the growth in hospital deliveries, is the increasing reliance on standardised procedures. This domination of formal procedures showed in midwifery training: 'Form ranked above everything else, including the well-being of mother and child. Form, indifferent as it might be to need, was the thing' (Armstrong and Feldman 1987: 27).
Midwifery practice
8.1 In midwifery practice pregnancy is a normal event in a woman's life cycle, which requires some special attention in the form of antenatal, perinatal, and postnatal care, but frequently this requirement results in fairly minimal monitoring, advice and support. Midwifery practice is subject to legal restrictions, since midwives in most countries are not allowed to conduct certain procedures (e.g. Caesarean Sections) or use certain instruments (e.g. forceps). Thus the description of midwifery practice is not based on what midwives do-everything midwives do falls under midwifery practice-but also what it should do based on its own underlying assumptions. One could try to describe the characteristics of the midwifery practice with the aid of a series of detailed accounts of pregnancy and labour (e.g.Oakley and Houd 1990: 68-80), but this does not solve the problem of overlap between 'midwifery practice' and 'women-centred ideology' completely (see below).8.2 Rothman (1982: 34) asserted that the midwifery practice tends to be a woman's perspective on birth, in which women are the subjects, the doers, and the givers of birth. The midwifery practice emphasizes normality, in order to justify non-medical control of the field of pregnancy and labour: e.g. 'a spontaneous delivery in the absence of detectable abnormality is a form of labour that can rarely be improved upon' (Zander et al. 1978: 122-3). In the US this approach involves elements of the holistic-health, back-to-nature movement, according to Rothman (1982: 34). Whilst Nordenfelt (1987: 113), in arguing that pregnancy is not an illness, but 'a necessary evil for the sake of a good end', still has a fairly limited mechanical approach to pregnancy, and does not regard it as a stage of personal growth and emotional fulfilment, as some adhering to midwifery practice do. The Royal College of Midwives (RCM 1991: 13) in the UK, by contrast, believes that during antenatal care: (a) greater priority should be given by all professionals to social and psychological aspects of pregnancy, and (b) much greater attention needs to be given to the discomforts pregnant women experience. Thus advocating more of a midwifery practice.
8.3 Kitzinger (1980: 2) wrote over two decades ago: 'Bringing new life into the world has always been one of the great acts with symbolic significance beyond the task of pushing an infant out of a female body.' A decade later she changed her caricature from a woman (actively) pushing to a baby (passively) being pulled out. 'For childbirth has much deeper significance than the removal of a baby like a decayed molar from a woman's body' (Kitzinger 1991: 8). What she referred to is, of course, the sense of power and active involvement of the pregnant woman. In many industrialised countries opting for a home birth can reflect a positive decision about the birth, unlike a hospital birth where a woman's role tends to be limited to deciding not to have certain procedures done to her. The experience of childbirth is seen as valuable in its own right in midwifery practice. Graham and Oakley (1986: 55) expressed this as follows: 'Though in almost all cases the goal of the live birth of a healthy infant is paramount, success means primarily a satisfactory personal experience.' The experience of the woman in childbirth is important. Even if the baby is not born alive, birth is still an important event (Oakley 1990:117). Or as Rothman (2001: 184) put it: 'Midwives, in contrast, ask a question that simply makes no sense in the medical model. If the baby is going to die anyway, then ask: "why spoil the pregnancy?"' A question Rothman (2001: 184) herself answered with anther question: 'Why indeed?' The place of delivery, or the wider issue of choice, became, in itself, an important part midwifery practice. Hospitals are not just institutions to help sick people, but they are also large-scale bureaucratic organisations dominated by medical professionals and managers who have their own interests. Zander et al. (1978: 122) listed protection from meddlesome medical intervention as one of the objectives of UK supporters of home births.
A continuum of working practices
9.1 Working practices are normally neither rigid-all working practice is somewhere in between two extreme ends of a continuum-nor static: individual practitioners or whole maternity units can change their working practice over time. Examples of the former are the range of working practices amongst midwives in Scotland (Askham and Barbour 1999;Murphy-Black 1992). Thus if maternity services providers were placed on this continuum most practices would be 'falling towards the middle' (Rooks 1999: 373). Stapleton (1997: 49) gave an example of change over time in midwifery practice as the exposure of deficiencies in the medical model had 'gradually encouraged the need for a more humane, women centred approach'. Whilst Porter (1999: 187) quoted studies which reported that midwives were no better than obstetricians at, for example, explaining procedures to women (Thomson 1994), or that views of obstetricians and midwives on pain relief were more likely to agree than that of midwives and the women under their care (Rajan 1993). Or as Foley and Faircloth (2003: 166) pointed out '..in practice (italic in original), the medical model is not simply an oppositional framework used for the discrediting of a holistic approach. Rather, it is a discursive resource that can be artfully used in the crediting of the profession of midwifery.'9.2 An example of changes occurring in working practice can be found among American lay midwives (i.e. midwives trained through apprenticeship). Lay midwives started out by presenting themselves as 'sisters' of their clients, practising at home, when legislation catalysed the change towards working in a more businesslike manner, '... the pressure was towards an increasingly conservative practice' (Reid 1989: 237.) Similarly, pregnant women's own childbirth definitions represent 'a continuum of beliefs rather than a dichotomy of natural versus medical' (Howell-White 1997: 934). Some women will welcome taking an active role whilst others will prefer to be passive and to leave decision-making to the health care provider (Too 1996). Furthermore, conflicting models of practice do not necessarily lead to conflicts in practice (Porter 1999: 148). In everyday working practice the different maternity service providers are complementary to each other, working towards 'collegiality, cooperation, communication, and complementarity-not competition' (Rooks 1983: 4).
9.3 One can envisage the obstetrical practice taken to its full extent, i.e. defining every pregnancy as an illness and treating every pregnant woman as a hospital patient under the care of an obstetrician. The following example, takes the model of midwifery practice to its logical conclusion. Damstra-Wijmenga (1984:427) found that two out of 1,692 women who gave birth in one Dutch city had chosen not to have any maternity care. They saw neither a doctor nor a midwife at any stage of pregnancy or delivery. It could be argued that the childbirth of these two women constitutes an extreme example of what Table 2 labelled midwifery practice, because there is no need for medical check-ups if one regards pregnancy and childbirth as a normal part in a woman's life cycle. It is a paradoxical feature of the proposed usage of terminology that if taken to its logical conclusion, 'midwifery practice', with its focus on normality and with the individual woman as an active participant, will not even have a midwife involved.
Ideological level
10.1 At the ideological level, claims are made to defend or propagate certain practices and discredit others. 'Ideology' as used in the sociology of knowledge, where ideas are regarded as socially determined and as reflecting socially located interests, without suggesting that a particular ideology is either true or false (Berger and Luckman 1966). Ideology always colours what one 'sees', for example, how one experiences, values approaches and describes a particular birth, midwifery consultation or antenatal visit.10.2 Ideology can be regarded as rhetorical, but not necessarily as uncritical of the subject's own way of working. Ideologies can be seen to be intolerant of alternatives, and to treat them as incompatible and inferior. Ideologies in that sense are similar to political dogma. Medical and social perspectives on pregnancy are not just views contradicting each other, but represent 'competing ideologies of reproduction' (Graham and Oakley 1986:50-74). As Edwards (2000: 70) commented: 'A dominant ideology, such as the medical approach to birth, assumes a monopoly on knowledge.' Whilst in midwifery members have 'developed conflicting ideologies that have been useful in determining the direction of the occupation' (Langton 1991: 171). Each has its own frame of reference, which embraces both the notion of an ideological perspective--a system of values and attitudes through which mothers and doctors view pregnancy--and of a reference group, consisting of a network of individuals, who have significant influence upon these sets of attitudes and values (Graham and Oakley 1986: 97).
10.3 It is the exclusive correctness of a certain approach that the person who makes the claim tries to establish, in order to win others over to this practice. This often means that assertions are being made which cannot be proven, and which derive their appeal from ideological commitments. Therefore, one should always bear in mind that ideology does not simply reflects social reality, but also influences and shapes it by helping it mobilise action on behalf of particular interests. The underlying ideology drove technological development in pregnancy and childbirth, according to Rothman (2001: 180).
The biomechanical ideology
11.1 Many medical professionals claim that one could be sure only in retrospect which pregnancy was low-risk and which was high-risk (Lumey 1993: 173), they subsequently claim that they can reduce that risk (DeVries 1993). Biomedicine must emphasize the disease-like nature of pregnancy, its 'riskiness', in order to justify medical interventionist management. Risk is not a neutral term, as Lane (1995: 57) pointed out 'Doctors do not talk about "good" risk.' Hence the view is often expressed that 'the "normality" of pregnancy and childbirth is a dangerous fallacy' (Oakley and Houd, 1990:30). DeVries and Barroso (1997: 268) argued that antenatal screening turns every pregnancy into a risky pregnancy, supporting the idea of many American obstetricians that "a pregnancy is low risk only in hindsight". Pregnancy in this ideology becomes 'a neoplastic, endoparasitic (i.e. neoparasitic) autoinfection of relatively high pathogenicity and low average virulence which is localized, self-limited, and nontransmissible' (Hern, 1975: 370). In addition, the biomechanical ideology incorporates the claim that it was 'medical research, technology and assistance that has brought down the maternal and infant mortality rates,' as obstetrician Roberts (1989: vi) wrote in her reply to the critics of medicalisation of childbirth.11.2 The American obstetrician, Cook, provided a graphic example of the tactic of establishing claims by de-legitimising the opposite view with his strong views about people who oppose obstetrical practice. For example, he attacked the critics of medicalisation of childbirth in the US as follows:
'the self-appointed, unlearned experts, seek to authenticate their own flawed point of view.... launch diatribes against everything they choose not to understand, would substitute pseudoscience, pop culture, and emotionalism for scientific care of the unborn and newborn.... They are dedicated people and have made a inestimable contributions to their cause-which is defamation and sensationalism' (Cook 1982: 6).
The women-centred ideology
12.1 The women-centred ideology stresses the normality of childbirth, e.g. 'Birth is a biosocial process which is, by its very nature, a feminine process and a sexual process' (Wagner 1986: 13-4). This ideology also emphasises how small the likelihood is of something going wrong, and moreover asserts that one should not just look at statistical chances but should assess each woman individually as a person. Thus, the editorial It's time to 'think different' about the art and science of midwifery in a recent US midwifery journal pronounced: 'Now is the time for us to lay claim to our own expressions of art and science, and contribute a long-absent perspective from the women's and family health and childbirth equation' (Paine 2001: 1). This ideology become in the 1970s what Macintyre (1977) called 'the myth of a golden age' of maternity care, in which 'women gave birth to healthy, happy babies with very little intervention other than the support of a kind and trusted midwife' (Porter 1999: 186). Since most industrial societies have a high hospital-birth rate, the women-centred ideology is often expressed in language that is (at least implicitly) anti-doctor and anti-hospital. Kitzinger (1990: 1) highlighted this as follows: 'When a woman questions dogmatic policies instituted by the medical establishment, takes on the responsibility of having a homebirth, and overcomes the obstacles that are put in her way, she is not just expressing an emotional preference.' Under such circumstances women would be voicing their opinion in the face of considerable pressure from health care providers (and possibly family), in other words: there is nothing romantic about it!12.2 The emotional bonding and the special link between the mother and the newborn are also stressed as part of a normal, but special event in human life. Thus childbirth activists make claims such as: 'Home birth is about love and attention' and that 'Doctors do not talk about love' (e.g. Van Teijlingen 1994: 318). Such claims contrast with rationalising (i.e. non-emotional) rhetoric of many biomedical experts. Note, too, that the discourse about mother-infant bonding has been seen as ideological by at least one feminist author (Eyer 1993).
12.3 The issue of choice in maternity care is tied in with the active involvement of the woman in the whole process of childbirth. With regard to the question 'Who controls childbirth?' Graham and Oakley (1986:55) emphasised 'a woman's capacity to sense and respond to the sensations of her body.' Control over childbirth ties in with issues of choice; the latter is often regarded as restricted in hospital. The range of choices offered by hospitals is seen as a set of options, which are often very similar, and all part and parcel of the obstetrical practice. British hospitals, for example, 'offer a wide range of medical procedures and drugs, but a normal birth (one that is allowed to take a physiological course without interference from routine technological interventions) may be quite difficult to arrange' (Beech 1987: 9).
12.4 One of the characteristics of the midwifery practice is that each woman is regarded as an individual, judged on her relevant strengths and weaknesses, rather than on the statistical chance of certain obstetrical and medical risks. Describing midwifery practice as one in which 'nothing' is considered routine and that the midwife's greatest challenge is to assess each situation individually, making clinical decisions along the way in partnership with the woman' (Kennedy and Lowe 2001: 92), is clearly an ideological claim. The last person any woman would want to look after them in childbirth would be someone who does not know and act upon the routine, for example, the standard signs for something going wrong. What is meant is, of course, that every woman is taken as an individual not a statistics in the health care system. Another clear ideological claim can be found in Savage (1986: vxi), when she explained that: 'as the risks in childbirth become smaller, statistical methods of predicting.... which woman will lose her baby have a limited use...if you look at each woman as an individual, and plan her care with her, you will get the best result.' In other words, the biomechanical ideology is passé, as the statistical methods have lost their power of prediction, which has made way for individual approach advocated in the women-centred ideology.
12.5 The women-centred approach is also political; the claim that birth is about power and control is an often-repeated statement. For example, claims are made that: 'Home birth is about power, i.e. who controls health?' One of the reasons why doctors use machinery is because they do not believe in women's bodies. In the US one third of all babies are 'cut out or pulled out' (Van Teijlingen 1994: 319). Note the violent language, something that can also be found in Kitzinger (1991: 8). Another key ideological claim of the women-centred approach is to 'natural' childbirth (e.g. Annandale 1988; Howell-White 1997). From this perspective midwifery should focus on things that are designed by nature and the word 'natural' should replace the word 'normal' in many contexts. 'Normal' is a word that comes from measurement and statistical probability (Bergstrom 1997: 420). A final element of a political claim is to overstate the virtues of one's own ideology. Thus Litoff (1986: 240) accused Rothman of presenting 'a somewhat exaggerated view of the medical model of childbirth.'
Paradoxes in ideological claims
13.1 Ideological claims are by definition absolute, thus some experts have the conviction that "birthing models are textually pure and mutually exclusive" (Shaw 2002: 141). The claims made by proponents of the biomechanical ideology about improving mortality rates can be reinterpreted by the consumers as implying that childbirth is now safer than ever, and therefore less likely to require active medical assistance. It is therefore important to bear in mind that in reality people borrow aspects from both perspectives, despite the fact that, logically, they are mutually exclusive. An example of elements of the two ideologies being combined without an obvious contradiction is found in the following statement: 'Whilst improved mortality and morbidity statistics have clearly provided a strong justification for the medical management of childbirth, they do not explain why medical control has not been relaxed as standards have risen' (Evans 1985: 117).13.2 Here claims of decreased mortality and morbidity come from the biomechanical ideology, whilst the issue of reducing medical control originate from a women-centred ideology. It could be argued that the obstetrical practice thus becomes a victim of its own success. Since: 'obstetricians, through the introduction of skill and science in this century, removed death from the childbed. Precisely because of modern obstetrics, the risk of childbirth has become so slight for the mother of today that safe delivery has become to be considered the normal order of things. And now, buoyed by this false optimism, the antihistorical rebels are praising Nature as the source of the present-day blessing of safe childbirth and denying the contributions, for mother and child, of obstetrics' (Cook 1982: 5). Furthermore, ideological claims, which stress the risk aspect of childbirth, and more importantly, the ability of the obstetrician to overcome and control this risk, have contributed to a stream of lawsuits (especially in the USA) against obstetricians and hospitals by disappointed parents (Cartwright and Thomas 2001: 221-222). However, going to court has also become more acceptable in the UK (e.g.Symon 2002). This in turn, has led to more conservative practice with an increasing reluctance to permit natural vaginal deliveries (Sakala 1993;Schuman and Marteau 1993: 117).
13.3 The use of ideologies is not just limited to practitioners claiming that what they do is the best for humanity. The power of ideological claims is often that they are endorsed or at any rate echoed both by professionals in other fields, academics and lay people. For example, Branca's (1977) claim that doctors and pregnant women were both determined to alter the ways of childbirth for the good of the pregnant woman. At this point, one of the confusions outlined above occurs. Branca's analysis of medical progress is in itself clearly affected by a biomechanical ideology, since she equates the doctor's taking over childbirth from the midwives with progress for the pregnant woman. Similarly, Porter (1999: 186) observed that in several recent texts 'uncaring males are depicted as expropriating midwifery from caring women'.
13.4 It is interesting that at the level of ideology, proponents of both sides expose each other's biases. Talking about the psychological trauma of older children seeing their new sibling 'come into the world', which can be part of family-centred midwifery practice, Cook (1982:108) argued that the effects of this experience cannot be known for decades, by which time 'sociologists, anthropologists, and psychologists will undoubtedly claim to have sorted it all out, one way or another, according to their biases.' Those professionals who provide ideological endorsement for the midwifery practice of childbirth can run into the same trouble as the supporters of the obstetrical practice. Their ideological claim that childbirth is natural can be translated by pregnant women as 'a process which will evolve naturally without any outside intervention', and therefore, potentially excludes the midwife.
Transitions from one ideology to another
14.1 Changes in ideological perspectives occur, although these changes require more adjustment from practitioners than simple changes in the working practice over time. One such change-over of ideological perspective has been analysed by Rothman (1983: 262-3) in her study of American nurse-midwives, whose initial 'ideas of what a home birth should and would be like ... were based on their extensive experience with hospital births.' Rothman (1983: 263) compared the transition from one ideology to another with 'scientists' switch from one paradigm to another-a "scientific" revolution in the words of Kuhn (1970). Rothman thus underscored the point made above that ideologies tend to be mutually incompatible.The analytical level
15.1 The analytical models of childbirth also provide us with radically contrasting views of childbirth and related health and women's issues. At this level the medical model and the social model of childbirth come very close to Weber's notion of an abstract 'ideal type', which is an analytical construct that serves as a measuring rod to determine the extent to which social institutions are similar and how they differ from some defined measure (Coser 1977). Thus the concept of ideal type is based on the notion that 'social phenomena, in virtue of their manifold and fluid nature, can be analysed solely in terms of the extreme forms of their characteristics, which can never be observed in their purity' (Mitchell 1979: 99-100). However, the ideal type it is not itself a description of an empirical reality (Mechanic 1968: 173), but 'an abstraction that comes from empirically observed regularities' (italics in original) (Corbetta 2003: 22). Thus at the analytical level the medical/social model approach can epistemologically be linked to interpretivism.15.2 The description of each ideal type may read very much like its ideology but without the incorporated value judgement endorsing the corresponding practice. Table 2 indicates that the emphasis on each of the three levels is similar; the difference lies in its manifestation. Thus where the analysis contained in the medical model stresses the risk element in itself, the biomechanical ideology adds the claim that the obstetrical practice can best improve the chances of a positive outcome. Or where the social model accentuates in its analysis the active role of women in childbirth, the women-centred ideology adds the claim that the midwifery practice is what can best stimulate the active involvement of the woman.
15.3 This dichotomy between the two models is often traced back to Descartes (Davis-Floyd 1987: 481) or even the ancient Greeks (Wagner 1986: 11; 1994: 27). One path involves Art, Quality, Subjectivity, Femininity, Intuition, and Mind (Emotion), while the other part of the medical dichotomy involves Science, Quantity, Objectivity, Masculinity, Logic and Body. The second path is dominant in the medical world in particular and in our culture in general, because of the increasing rationalisation in society. At the analytical level, students of society can use the medical and social models alike as sociological tools for understanding developments in our society. They serve this purpose by encouraging us to give salience to features of the social world, which are especially relevant to whichever analytical model is uppermost at a given stage in our analysis. This allows us to study (a) those who have internalised a specific outlook on life; or (b) the dominant image of taken-for-granted approach to childbirth in society.
15.4 The medical model regards pregnant women as passive and as patients. Rothman (2001: 184) argued that the medical model of pregnancy is 'both product oriented and fetocentric.' Pregnant women, women in labour and new mothers lack the knowledge or authority to decide on medical treatment, not only with regard to clinical risks during labour, but also in the postnatal period. When seen within the framework of the medical model, the pregnant woman comes to be viewed in mechanistic terms as a patient, almost as an object. 'Birthing women are thus objects upon whom certain procedures must be done' (Rothman 1982: 34). When one is working with a medical model, one tends to focus on the directly intended functions of technology used for monitoring fetal growth, rather than on the fact that this technology can in certain circumstances be used to bring pressure to bear on the pregnant woman. As Martin (1989:145) has pointed out: 'Doctors, husbands, and state governments are successfully using legal sanctions to force women to involuntarily alter their diets (stop taking drugs), alter their daily activity (be confined to a hospital for the last weeks of pregnancy), or undergo Cesarean section to protect the rights of the fetus.'
15.5 The working practice and the ideology put forward by doctors does not seem to be based simply on their reliance on the definition of the risk involved in pregnancy, but also on a certain rather one-sided emphasis in the medical model's implied analytical perspective on the role of women in society. The medical model corresponds at an analytical level to the ideologically dominant view of medicine in general and of childbirth in particular in our society, in that within this framework one will tend to pay little attention to the potentially coercive features of medical technology in childbirth.
15.6 The social model emphasises the fact that pregnancy and labour are in principle, and often in practice, normal physiological processes. Moreover, it starts from the premise that for a woman having a baby often changes not just her medical status, but also her social roles, e.g. 'becoming a mother' (Oakley 1979; Rooks 1999), and her social status, for instance, it can mean a lower income, losing a job, increased financial dependency on partner, parents, and social welfare benefits. Ball (1987: 27) added: 'The birth of a new human being is an intensive personal, emotional and family-centred event.' In the social model, 'women are not compared to a hypothetically stable, noncycling male system but are expected always to be in one or another phase of reproductive life.' (Rothman 1982: 156.) By contrast, the medical model shows us pregnancy and birth from the perspective of society's technological preoccupation, and in that sense through men's eyes (Rothman 1982: 34). Rothman thus incorporates gender within the social analysis of childbirth.
Incommensurability of analytical models
16.1 At the analytical level, the medical and social models of childbirth are ultimately incommensurable, what Comaroff (1977) has called the 'conflicting paradigms of pregnancy'. But rather than dwelling on the associated conflicts, sociologists should dwell on the way the fundamental concerns which underlie these two models are focused on quite distinct aspects of childbirth. It is not so much that they clash with each other, as that neither of them directly addresses the issues that are central to the other. That is, they present distinctive images of reality.16.2 It has been argued that the unique perspective and practice of the midwifery profession provides a basis for bringing together the medical definition and the social definition of birth, 'to provide balance in the health care system... However, present-day midwifery in the industrialised world does not fulfil this role' (Page 1988: 251-2). She listed five principles for both doctors and midwives to adhere to in modern midwifery care: (a) continuity of care; (b) respect for the normal; (c) enabling informed choice; (d) recognition of birth as more than a medical event; and (e) family-centred care (Page 1988: 252-60.) Page's principles are very similar to those ascribed to midwifery practice, and, at the same time, they read like a summary of the women-centred ideology. Thus a change in working practice towards midwifery practice will change the balance in the health care system. However, she implies that the medical and social model can somehow be amalgamated into a new midwifery model at the analytical level. However, such changes in the working practice will not change the analytical model. In other words, changes in a complex reality do not necessarily imply changes in the less complicated analytical tools. We can analyse the new situation and find that it contains more elements of a social model than a medical model. Page's approach illustrates that confusion is liable to occur when the levels of practice, ideology and analysis are not separated.
16.3 Neither an obstetrical nor a midwifery-based approach to childbirth practice is static. Both contribute to a wider process wherein situations are being continually redefined in ideological terms. As this occurs, the ideological claims put forward play an important role in explaining the new situation. At the same time, ideological claims are made that the new way of practising is now the 'correct' way. The analytical models are slower to change than either working practice or their corresponding ideologies, since an analytical model is based on more fundamental underlying presuppositions concerning, for example, the definition of the nature of pregnancy. Though individual people may change their minds about the definition of pregnancy, and may consequently change their working practice and ideology, the underlying presuppositions remain substantially unchanged at the analytical level. Nevertheless, even these presuppositions are not in principle incapable of evolving in response to accumulating evidence regarding what is safe or what is psychologically beneficial. This would eventually alter the content of the medical model.
16.4 Thus in everyday life institutional changes typically take place either in the working practice, or in the ideology or both. Certainly, individual practitioners sometimes change their minds after experiencing the other working practice, or after re-examining the 'evidence'. However, over and above this kind of individual change of perspective, more wide-ranging changes are taking place and have taken place in the social organisation of maternity care. Gradually, one established working pattern is replaced by a quite different working pattern. A substantial change in working practice is accompanied by a change of ideology, for example the move from home birth to hospital birth during the twentieth century meant that midwifery practice in the UK is now largely hospital based. This redefining of the situation is required for the purpose of legitimating the new working practice.
Limitations of the social/medical model dichotomy
17.1 We must bear in mind that biomedicine is still the dominant paradigm in modern health care (Gillespie and Gerhardt 1995: 81) including preventative medicine (Bengel et al. 1999: 17). Often the social model is contrasted with the medical model, as Kelly et al. (1997: 355) reminded us, therefore both models are 'united by the commitment to the existence of a system that is capable of being destroyed, broken down and analysed'. The social model is based on a belief that, behind the surface manifestations of disease, lie 'real' causes relating to the way in which society is organised and structured (Gillespie and Gerhardt 1995: 82). However, some (especially post-modernists) have criticised the underlying principles of a sociological analysis, which includes medical and social models, especially when linked to notions of social engineering. From a postmodernist perspective the practice of social theory, i.e. attempts to intervene in and control social forces and relations, is no longer relevant or useful (Maynard 2001: 110). Taking a postmodernist stance there is no possibility of deciding what the real needs are of patients, pregnant women, doctors, or anybody else. Although taking a sceptical approach to postmodernism we must be open to some of the interesting and exciting issues it raises (Maynard 2001: 111).Conclusion
18.1 Sociologists take pride in making a problem out of the 'taken-for-granted' notions in society. We must do the same with our tools and concepts. The medical model has become a taken-for-granted concept both within sociology and the wider world of academia and practice. One source of confusion here is that there are three different levels at which one can operate when comparing and contrasting a social and medical model. These levels sometimes overlap, and are difficult to disentangle. As a result, students of childbirth are liable to fall into the trap of simply describing a working practice and/or propounding its associated ideology rather than adopting an analytical approach to the issue.18.2 People readily move on from their way of applying their particular way of childbirth practice to creating a justification for this practice in the form of an ideology. Rose (1982) distinguished between the concepts used by participants in navigating their way through their social worlds, and theoretical concepts constructed by researchers. The originally theoretical concept of the medical model has also become an easy-to-use lay concept. This paper has disentangled the concept as used by non-sociologists (i.e. at level of practice and/or ideology) from that belonging solely to the analytical level. The uncritical use of the concept 'medical model', i.e. using the practical and/or ideological levels as if these are pure analytical concepts is detrimental to sociology. If sociologists are not careful with their tools and let others use them uncritically, we run the risk of having to work with rather blunt tools ourselves. Therefore, it is important that we make a clear theoretical distinction between the three different levels of analysis.
Acknowledgements
Many thanks to Dr. Peter McCaffery for comments and suggestions on earlier drafts; Ms. Jillian Ireland for comments on the final draft; and the anonymous reviewers for Sociological Research Online for their helpful comments on the original submission.References
ANNANDALE, E.C. (1988) 'How midwives accomplish natural birth: Managing risk and balancing expectations', Social Problems, Vol. 35, No. 2, pp. 95-110.ARMSTRONG, P. and FELDMAN, S. (1987) The Gentle Art: A Midwife's Story. London: Corgi Books.
ARNEY, W.R. (1982) Power and the Profession of Obstetrics. Chicago: University of Chicago.
ASKHAM, J. and BARBOUR, R.S. (1999) 'The role and responsibilities of the midwife in Scotland' in: E. van Teijlingen, G. Lowis, P. McCaffery, and M. Porter (editors) Midwifery and the Medicalization of Childbirth: Comparative Perspectives, New York: Nova Science.
BALL, J.A. (1987) Reactions to motherhood: The role of post-natal care. Cambridge: Cambridge University Press.
BARROWS, D.C. (1998) 'The community orientation of social model and medical model recovery programs', Journal of Substance Abuse Treatment, Vol. 15, No. 1, pp. 55-64.
BECKER, G. and NACHTIGALL, R.D. (1992) 'Eager for medicalisation: the social production of infertility as a disease', Sociology of Health and Illness, Vol. 14b, No. 4, pp. 456-471.
BEECH, B. L. (1987) Who's having your Baby?: A Health Rights' Handbook for Maternity Care. London: Camden Press.
BENGEL, J., STRITTMATTER, R. and WILLMANN, H. (1999) 'What Keeps People Healthy? The Current State of Discussion and the Relevance of Antonovsky´s Salutogenic Model of Health', Research and Practice of Health Promotion Vol. 4, Cologne: Federal Centre for Health Education. http://www.bzga.de/bzga_stat/fachpubl/pdf-datei/efh04.pdf
BENOIT, C. (1989) 'The professional socialisation of midwives: Balancing art and science', Sociology of Health and Illness, Vol. 11, No.2, pp.160-80.
BERGER, P.L. and LUCKMAN, T. (1966) The Social Construction of Reality. Harmondsworth: Penguin.
BERGSTROM, L. (1997) 'Midwifery as a discipline', Journal of Nurse-Midwifery, Vol. 42, No. 5, pp. 417-20.
BRANCA, P. (editor) (1977) The Medicine Show: Patient Physician and the Perplexities of the Health Revolution in Modern Society. New York: Science History.
BRYAR, R.M. (1995) Theory for Midwifery Practice. London: Macmillan.
CARTWRIGHT, E. and THOMAS, J. (2001) 'Constructing Risk: Maternity care, law, malpractice', in R. DeVries, C. Benoit, E.R. van Teijlingen and S. Wrede (editors) Birth by Design: Pregnancy, maternity care , and midwifery in North America and Europe, New York: Routledge.
CHANG, V.W. and CHRISTAKIS, N.A. (2002) 'Medical modelling of obesity: a transition from action to experience in a 20th century American medical textbook', Sociology of Health and Illness, Vol. 24, No. 2, pp. 151-77.
CHILD, N. (2000) 'The limits of the medical model in Child Psychiatry', Clinical Child Psychology and Psychiatry, Vol. 5, No.1, pp.11-21.
COMAROFF, J. (1977) 'Conflicting paradigms of pregnancy: Managing ambiguity in antenatal encounters', in A. Davis and G. Horobin (editors) Medical encounters: The experience of illness and treatment. London: Croom Helm.
CONRAD, O. and SCHNEIDER, J.W. (1980) 'Looking at levels of medicalization: A comment on Strong's critigue of the thesis of medical imperialism', Social Science and Medicine Vol. 14A, pp. 75-79.
COOK, W.A. (1982) Natural Childbirth: Fact and Fallacy. Chicago: Nelson-Hall.
CORBETTA, P. (2003) Social Research: Theory, Methods and Techniques. London: Sage.
COSER, L.A. (1977) Masters of Sociological Thought: Ideas in Historical and Social Context, (2nd Edn) New York: Harcourt Brace Jovanovich.
CRONENWETT, L. and BRICKMAN, P. (1983) 'Models of helping and coping in childbirth', Nursing Research vol. 32, no.2, pp.84-88.
DAMSTRA-WIJMENGA, S.M.I. (1984) 'Home confinements: the positive results in Holland', Journal of the Royal College of General Practitioners, Vol. 34, pp. 425-430.
DAVIS-FLOYD, R. (1987) The technological model of birth, Journal of American Folklore. Vol. 100, No. 398, pp. 479-495.
DAVIS-FLOYD, R. and SARGENT, C.F. (editors) (1997) Childbirth and Authoritative Knowledge: Cross-Cultural Perspectives. Berkeley: University of California Press.
DEVRIES, R.G. (1993) 'A cross-national view of the status of midwives'. In: E. Riska and K. Wegar (editors) Gender, work and Medicine: Women and the medical division of labour. London: Sage.
DEVRIES, R. and BARROSO, R. (1997) 'Midwives among the machines: Re-creating midwifery in the late twentieth century', in: H. Marland and A.M. Rafferty (editors) Midwives, Society and Childbirth: Debates and controversies in the modern period. London: Routledge.
EDWARDS N.P. (2000) 'Women planning homebirths: Their view own views on their relationships with midwives', in: M. Kirkham (editor) The midwife-mother relationship. Houndsmill: Macmillan Press Ltd.
EVANS, F. (1985) 'Managers and labourers: women's attitudes to reproductive technology', in: W. Faulkner and E. Arnold (editors) Smothered by invention: technology in women's lives. London: Pluto Press.
EYER, D. (1993) Mother-Infant Bonding: a scientific fiction. New Haven, Connecticut: Yale University Press.
FLEMING, V.E.M. (1998) Women-with-midwives-with-women: a model of interdependence. Midwifery, Vol. 14, No. 3, pp. 137-143.
FOLEY, L and FAIRCLOTH, C.A. (2003) 'Medicine as discursive resource: legitimation in the work narratives of midwives', Sociology of Health and Illness, Vol. 25, No. 2, pp. 165-184.
FREIDSON, E. (1970) Profession of Medicine, a Study of the Sociology of Applied Knowledge. New York: Harper and Row.
GERARD, J.B. (1999) 'The medical model of mental illness: Its application to the insanity defence', International Journal of Law and Psychiatry, Vol. 22, No.1, pp.65-78.
GILLESPIE, R. and GERHARDT, C. (1995) 'Social dimensions of sickness and disability' in G. Moon and R. Gillespie (editors) Society & Health: An introduction to social science for health professionals. London: Routledge.
GRAHAM, H. and OAKLEY, A. (1986) 'Ideologies of reproduction', in: C. Currer and M. Stacey (editors.) Concepts of health and illness and disease: A comparative perspective. Leamington Spa: Berg.
HELMAN, C.G. (1985) 'Communication in primary care: the role of patient and practitioner explanatory models', Social Science and Medicine, Vol. 20, No. 9, pp. 923-931.
HERN, W.M. (1975) 'The illness parameters of pregnancy', Social Science and Medicine, vol. 9, pp.365-372.
HOWELL-WHITE, S. (1997) 'Choosing a birth attendant: The influence of a woman's childbirth definition', Social Science and Medicine, Vol. 45, No. 6, pp. 925-936.
KELLY, M.P., DAVIES, J.K. and CHARLTON, B.G. (1997) 'Healthy cities: a modern problem or a post-modern solution', in M. Sidell, L. Jones, J. Katz and A. Peberdy (editors) Debates and Dilemmas in Promoting Health: A Reader. Houndsmills, Basingstoke: Macmillan Press Ltd.
KENNEDY, H.P. and LOWE, N.K. (2001) 'Science and midwifery: Paradigms and paradoxes', Journal of Midwifery and Women's Health, vol. 46, no. 2, pp.91-97.
KILLUS, J. (1984) Geburtsmethoden: Eine Orientierungshilfe (In German: Birth Methods: An introduction). Berlin: Rotation Verlag.
KITZINGER, S. (1980) Birth at Home. Oxford: Oxford University Press.
KITZINGER, S. (1990) Editorial, International Home Birth Movement (British Section Newsletter), Vol. 1, No.1, pp. 1-3.
KITZINGER, S. (1991) Homebirth and other alternatives to hospital. London: Dorling Kinderley.
KLOOSTERMAN, G.J. (1978) 'The Dutch System of home births', in S. Kitzinger and J. Davis (editors) The Place of Birth. Oxford: Oxford University Press.
KUHN, T.S. (1970) The Structure of Scientific Revolutions, Chicago: Chicago University Press.
LANE, K (1995) 'The medical model of the body as a site of risk: a case study of childbirth', in J. Gabe (editor) Medicine, Health and Risk. Oxford: Blackwell.
LANGTON, P.A. (1991) 'Competing occupational ideologies, identities, and the practice of nurse-midwifery', Current Research on Occupations and Professions Vol. 6, 149-177.
LAZARUS, E. (1997) 'What do women want? Issues of Choice, Control, and Class in American Pregnancy and Childbirth' in R. Davis-Floyd and C.F. Sargent (editors) Childbirth and Authoritative Knowledge: Cross-Cultural Perspectives. Berkeley: University of California Press.
LICHTMAN, R. (1999) 'Medical models and midwifery: the cultural experience of birth', in: E. van Teijlingen, G. Lowis, P. McCaffery and M. Porter (editors) Midwifery and the Medicalization of Childbirth: Comparative Perspectives, New York: Nova Science.
LITOFF, J.B. (1986) The American Midwife Debate: a Sourcebook on its Modern Origins. New York: Greenwood Press
LOWIS, G.W. and MCCAFFERY, P.G. (1999) 'Sociological factors affecting the medicalization of midwifery', in: E. van Teijlingen, G. Lowis, P. McCaffery and M. Porter (editors) Midwifery and the Medicalization of Childbirth: Comparative Perspectives, New York: Nova Science.
LUMEY, L.H. (1993) 'Illness versus Natural Process: Competing Paradigms in Great Britain and the Netherlands', in E. Abraham-Van der Mark (editor) Successful Home Birth and Midwifery: The Dutch Model. Westport, Connecticut: Bergin & Garvey.
MACINTYRE, S. (1977) 'The myth of the golden age', World Medicine, Vol. 12, (Issue June 15), pp. 17-22.
MECHANIC, D. (1968) Medical Sociology: A selective view. New York: The Free Press.
MITCHELL, G.D. (1979) A New Dictionary of Sociology. London: Routledge & Kegan Paul.
MARTIN, E. (1989) The Woman in the Body: A Cultural Analysis of Reproduction. Milton Keynes: Open University Press.
MAY, C. (2001) 'Pathology, identity and the social construction of alcohol dependence', Sociology, vol.35, no.2, pp.385-401.
MAYNARD, M. (2001) 'Feminism and postmodernism in social theory' in R.G. Burgess and A. Murcott (editors) Developments in Sociology, Harlow: Pearson Education Limited.
MURPHY-BLACK, T. (1992) A Survey of Systems of Midwifery Care in Scotland. Edinburgh: University of Edinburgh, Nursing Research Unit.
NASH, A. and NASH J.E. (1979) 'Conflicting interpretations of childbirth: The medical and natural perspectives', Urban Life, Vol. 7, No. 4, pp.493-512.
NORDENFELT, L. (1987) On the Nature of Health: An Action-Theoretic Approach. Dordrecht, the Netherlands: D. Reidel Publishing Company.
OAKLEY, A. (1979) Becoming a Mother. Oxford: Martin Robertson.
OAKLEY, A. (1980) Women Confined: Towards a Sociology of Childbirth. Oxford: Martin Robertson.
OAKLEY, A. (1984) The Captured Womb: A History of the Medical Care of Pregnant Women. Oxford: Basil Blackwell.
OAKLEY, A. (1999) 'Who cares for women? Science versus love in midwifery today', in E. van Teijlingen, G. Lowis, P. McCaffery and M. Porter (editors) Midwifery and the Medicalization of Childbirth: Comparative Perspectives, New York: Nova Science.
OAKLEY, A. and HOUD, S. (1990) Helpers in Childbirth: Midwifery Today, London: Hemisphere Publishing Corporation.
OLDMAN, C. (2002) 'Later life and the social model of disability: a comfortable partnership?, Ageing & Society, Vol. 22, pp. 791-806.
PAGE, L. (1988) 'The Midwife's Role in Modern Health Care', in S. Kitzinger (editor) The Midwife Challenge. London: Pandora.
PAINE, L., L. (2001) It's time to 'think different' about the art and science of midwifery, Journal of Midwifery and Women's Health, Vol. 46, No. 1, p.1.
PORTER, M. (1999) 'The midwife in contemporary industrialised society', in: E. van Teijlingen, G. Lowis, P. McCaffery and M. Porter (editors) Midwifery and the Medicalization of Childbirth: Comparative Perspectives, New York: Nova Science.
RAJAN, L. (1993) 'Perceptions of pain and pain relief in labour: the gulf between experience and observation', Midwifery, Vol. 9, No. 3, pp.136-45.
REID, M. (1989) 'Sisterhood and Professionalisation: A Case Study of the American Lay Midwife', in S.C. McClain (editor) Women as Healers: Cross-Cultural Perspectives. New Brunswick: Rutgers University Press.
ROOKS, J. (1983) 'The context of nurse-midwifery in the 1980s: our relationships with medicine, nursing, lay-midwives, consumers and health care economist', Journal of Nurse-midwifery, Vol. 28, No. 5, pp.3-8.
ROOKS, J.P. (1999) 'The midwifery model of care', Journal of Nurse-midwifery, Vol. 44, No. 4, pp.370-374.
ROSE, G. (1982) Deciphering Social Research. London: Macmillan.
ROSENGREN, W.R. (1962) 'Social instability and attitudes toward pregnancy as a social role', Social Problems, Vol. 9, No. 4, pp. 371-378
ROTHMAN, B.K. (1982) In Labor: Women and the Power in the Birthplace. New York: W.W. Norton and Company.
ROTHMAN, B.K. (1983) 'Midwives in transition: the structure of a clinical revolution', Social Problems, Vol. 30, No. 3, pp.261-271.
ROTHMAN, B.K. (2001) 'Spoiling the pregnancy: Prenatal diagnosis in the Netherlands', in R. DeVries, C., Benoit, E. van Teijlingen and S. Wrede (editors) Birth by Design: Pregnancy, Midwifery Care and Midwifery in North America and Europe, New York: Routledge.
SAKALA, C. (1993) 'Midwifery care and out-of-hospital birth settings: how do they reduce unnecessary cesarian section births?', Social Science and Medicine, Vol. 37, No. 10, pp.1233-1250.
SAVAGE, W. (1986) A Savage Enquiry: Who controls childbirth? London: Virago.
SCHUMAN, A.N. and MARTEAU, T.M. (1993) 'Obstetricians' and midwives' contrasting perceptions of pregnancy', Journal of Reproductive and Infant Psychology, Vol. 11, No.2, pp.115-118.
SHAW, R. (2002) 'The ethics of the birth plan in childbirth management practices', Feminist Theory, Vol. 3, No.2, pp.131-149.
STAPLETON, H. (1997)'Choice in the face of uncertainty', in M.J. Kirkham and E.R. Perkins (editors) Reflections on Midwifery, London: Baillière Tindall.
SYMON, A. (2002) 'The significance of time factors in cerebral palsy litigation', Midwifery, Vol. 18, No. 1, pp. 35-42.
TEIJLINGEN VAN, E.R. (1994) A social or medical model of childbirth? Comparing the arguments in Grampian (Scotland) and the Netherlands. Unpublished PhD, Aberdeen, UK: University of Aberdeen.
TEIJLINGEN VAN, E. and BRYAR, R. (1996) 'Selection guidelines for place of birth', Modern Midwife, Vol. 6, No. 8, pp. 24-27.
TEIJLINGEN VAN, E.R. (2003) 'Dutch Midwives: The Difference between Image and Reality' in S. Early & G. Letherby (editors) Gender, Identity and Reproduction: Social Perspectives. London: Palgrave.
THOMSON, A. (1994) 'Research into some aspects of care in labour', in S. Robinson and A. Thomson (editors) Midwives, Research and Childbirth Vol. 3, London: Chapman and Hall.
TOO, S. (1996) 'Do birth plans empower women? A study of their views', Nursing Standard, Vol. 10, No. 3, pp. 33-37.
WAGNER, M. (1986) 'The medicalisation of birth', in Claxton, R. (ed.) Birth Matters: Issues and Alternatives in Childbirth. London: Unwin Paperbacks.
WAGNER, M. (1994) Pursuing the Birth Machine: The search for appropriate technology. Camperdown, NSW, Australia: ACE Graphics
ZANDER, L., LEE-JONES, M. and FISHER, C. (1978) 'The role of the primary health care team in the management of pregnancy', in S. Kitzinger and J. Davis (editors) The Place of Birth. Oxford: Oxford University Press.